Dr. Kumaran A/L Krishnan, Ainul Arina Madhiah Bt Mohd Noor and Dr. Siti Salmah Binti Noordin
Kluster Perubatan Regeneratif, Institut Perubatan dan Pergigian Termaju (IPPT), USM
The history of ABO blood group ways back to 1901 when it was discovered by Karl Landsteiner. Landsteiner discovered the ABO blood group system by mixing the red cells and serum of each of his staff. He demonstrated that the serum of some people agglutinated the red cells of others. He identified three types, namely A, B, and C (C was later to be re-named O for the German “Ohne”, meaning “without”, or “zero”, “null” in English). A total of 43 human blood group systems are recognized and established by the International Society of Blood Transfusion (ISBT) as of today. However, ABO and Rh blood group systems remain the most essential. Blood groups are inherited and represent the contribution from both parents. ABO blood type is controlled by a single gene and is located on the long arm of ninth chromosome.
Detection of blood group is determined by the presence of antigens on the red blood cells and antibodies in plasma. Antigens are protein molecules found on the surface of red blood cells whereas antibodies are part of the defense mechanism which will recognize foreign substances and destroy them.
The ABO system has four main blood groups. Blood group A has A antigens on the red blood cells and has anti-B antibodies in plasma. Blood group B has B antigens with anti-A antibodies in plasma. Blood group AB has both A and B antigens, but no antibodies. Lastly, blood group O has no antigens but has both anti-A and anti-B antibodies in the plasma. Even though the ABO antigens are detectable at birth, however, they are only fully developed by 2-4 years of age. In contrast, the ABO antibodies are only detectable at 3-6 months of age and fully developed at 5-10 years of age. However, the ABO antibodies levels begin to decline in the elderly.
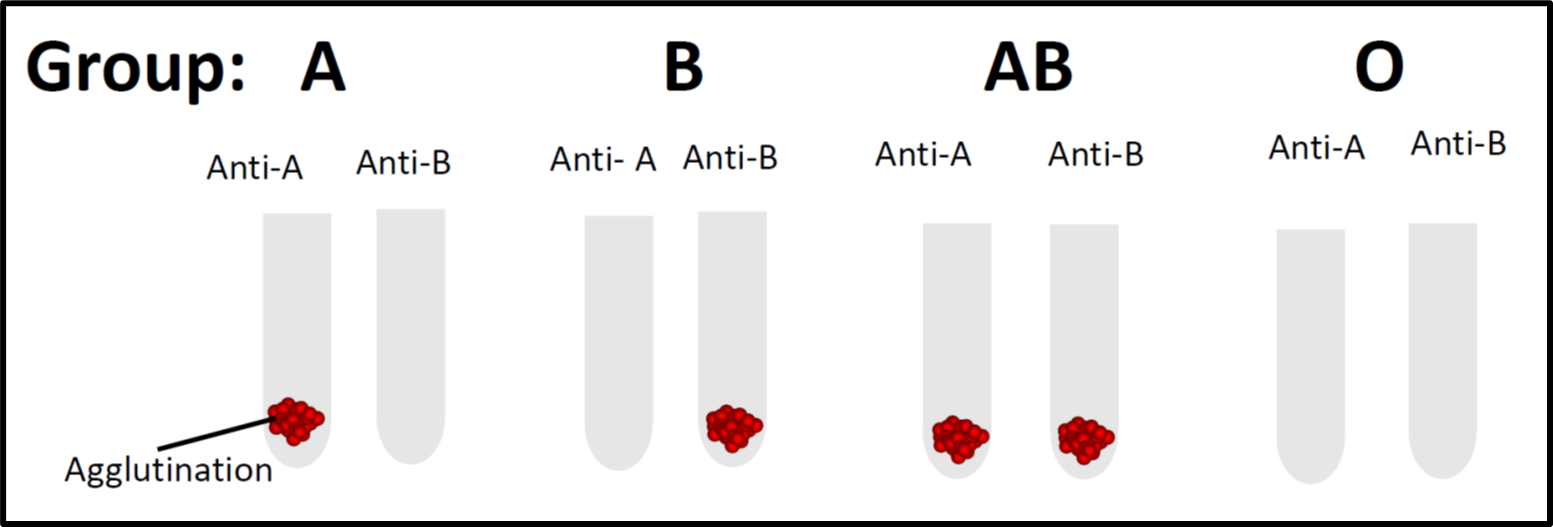
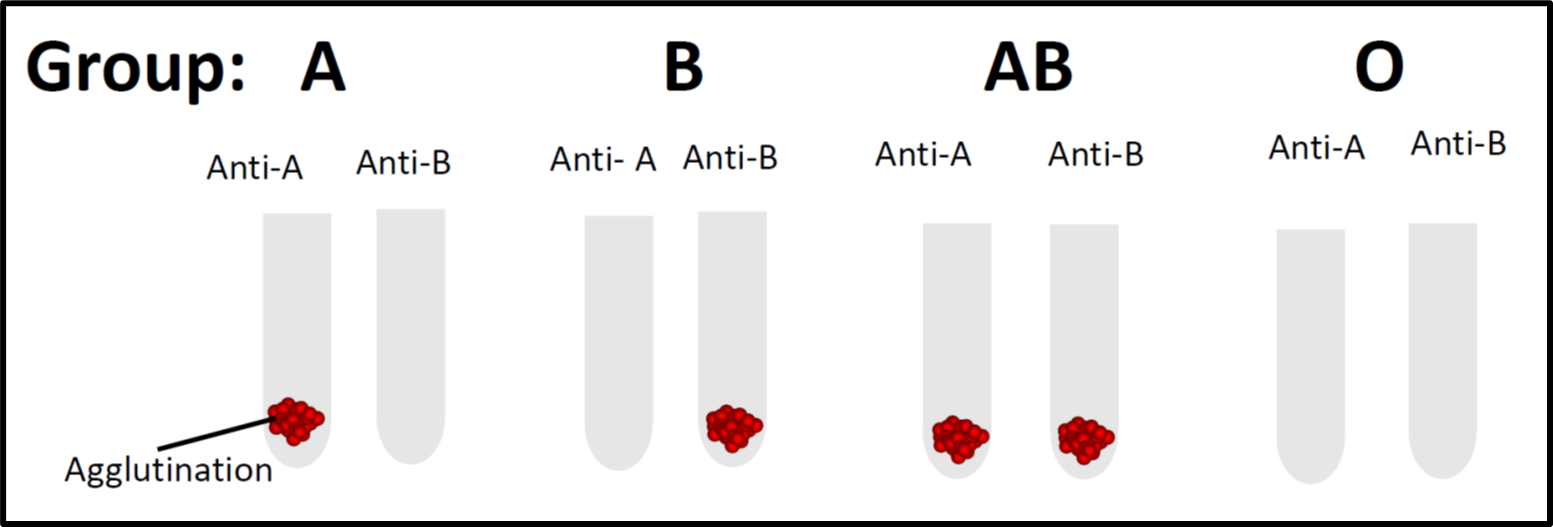
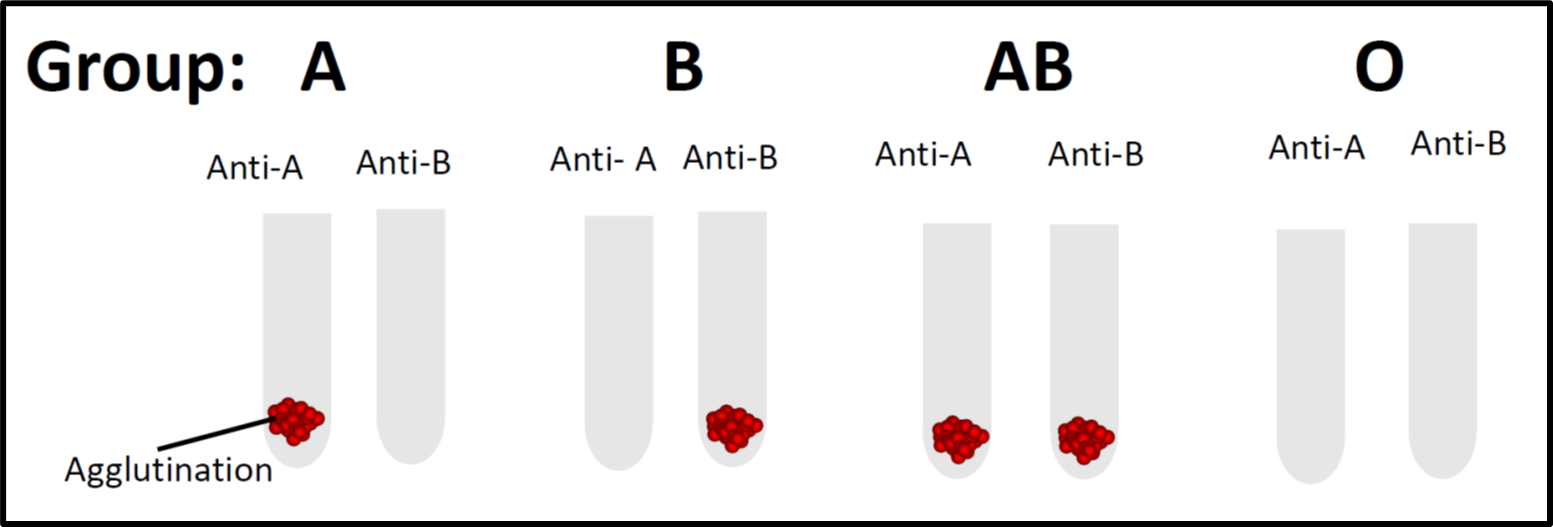
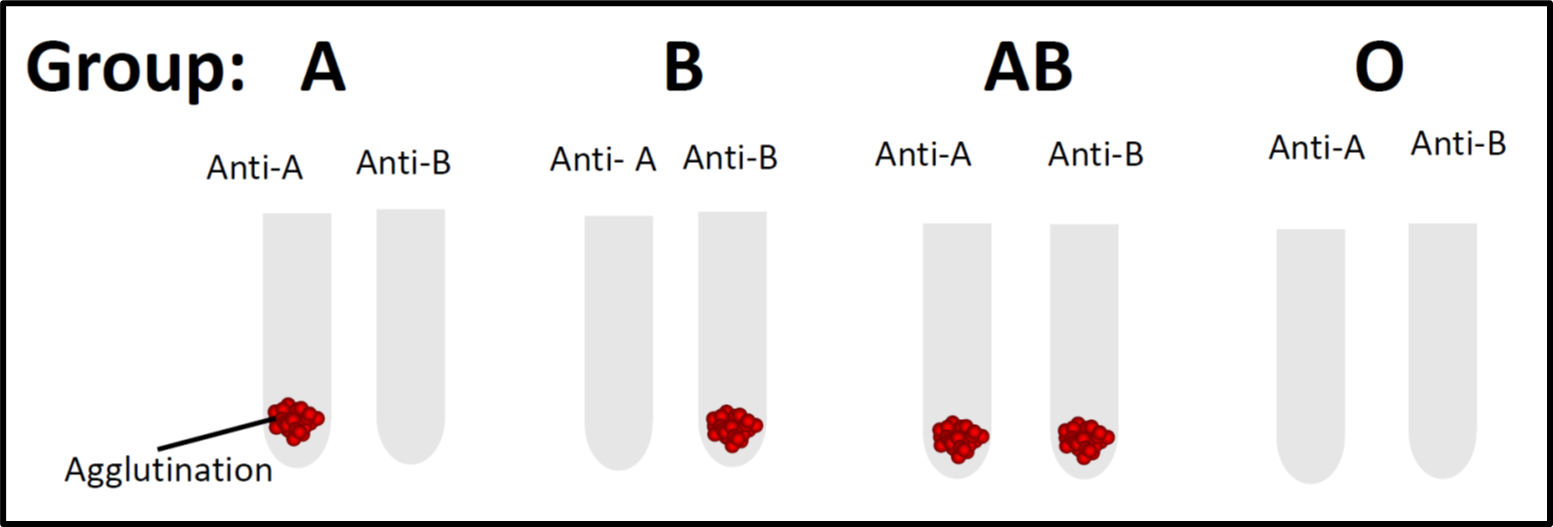
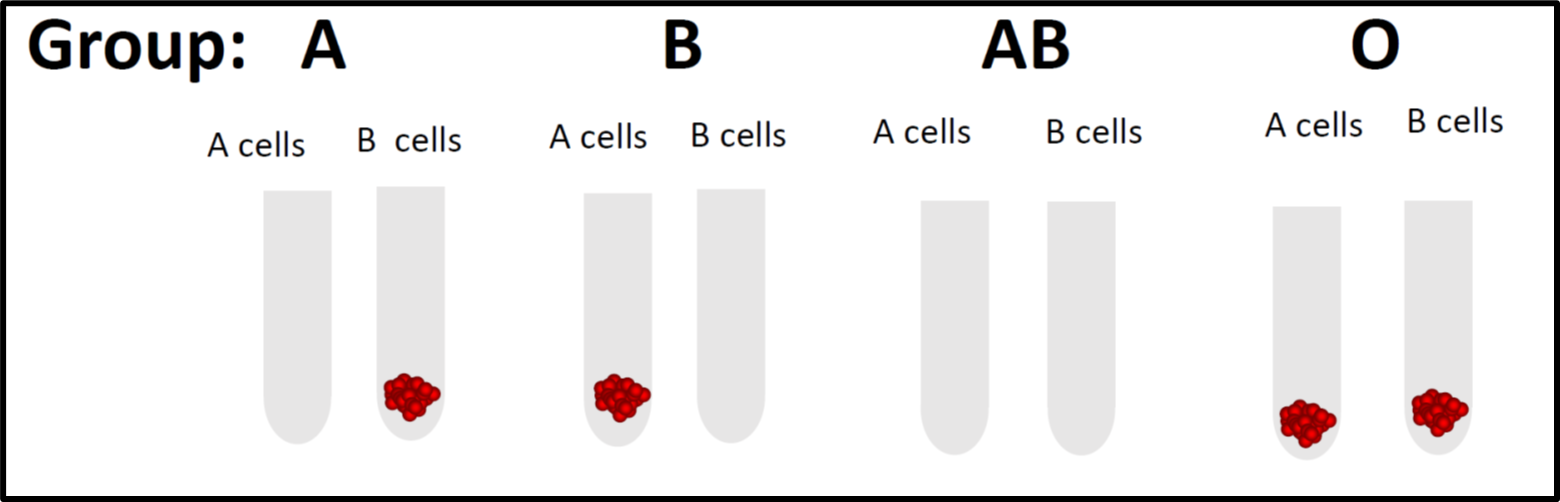
In most laboratories, blood group testing is performed by using forward and revere grouping. This test is usually conducted at room temperature (20-24 ?C). Forward grouping is performed by adding the patient’s red cells to commercialized reagent antisera (anti-A, anti-B, or anti-A,B) whereas reverse grouping is performed by adding the commercialized reagent red cells (A1 or B red cells) with the patient’s serum or plasma. For instance, if the patient’s red cells react with antisera-A in forward grouping and the patient’s serum reacts with B cells in the reverse grouping, it indicates that the patient is blood group A. However, there are instances where the ABO blood grouping showed a discrepancy between both forward and reverse grouping, thus further laboratory investigation will be needed. Such occurrence may be due to weak, missing, or extra antigens or extra antibodies.
Blood group O is the most common among Malaysians (34.5% among Malays, 38.3% among Chinese, and 36.7% among Indians). Receiving blood from the wrong ABO group can be life-threatening. For example, if a patient with blood group A is transfused with red cell group B, the anti-B antibodies in the patient will destroy the transfused B cells and this could lead to acute hemolytic transfusion reaction with a detrimental outcome. Nevertheless, individuals with blood group O are known as universal red cells donor and individuals with blood group AB are the universal plasma donors.
Figure 1: Forward blood grouping whereby commercialized reagent antisera is added to the tested red cells.
Figure 2: Reverse grouping whereby commercialized reagent red cells are added to the tested plasma.
Penulis Artikel
Nama penulis:
Dr Kumaran A/L Krishnan, Dr Ainul Arina Madhiah Bt Mohd Noor, Dr Siti Salmah Binti Noordin
Afiliasi:
Kluster Perubatan Regeneratif
Bidang kepakaran:
Transfusi Perubatan.