First day of as online course participant using Microsoft Teams platform.
This article is about the key lessons that I learned from participating virtually in Human and Veterinary Vaccinology course conducted by the University of Oxford, UK from October 23rd to 27th, 2023. The course utilized Microsoft Teams for live online teaching sessions, while additional materials and discussions were facilitated through Canvas, the university's virtual learning platform. Unfortunately, despite my engagement in the live online sessions, I was unable to join the in-person tours of the Pirbright Institute laboratories and Centre for Veterinary Vaccine Innovation and Manufacturing on the third day due to security concerns. That privilege was for participants who were physically present. You can read about the tours from an article written by Dr Asmida Isa who physically attended the course here https://news.amdi.usm.my/fullnews.php?id=aVgxWlVIWDNPamRlWHdpRVdkMVNxZz09.
My participation was sponsored by the National Institute of Biotechnology Malaysia (NIBM) as part of the National Vaccine Development Roadmap (PPVN) initiative by the Malaysian government aimed at cultivating more vaccine scientists. The attendees comprised academics, researchers from private laboratories, healthcare professionals, and individuals involved in vaccine promotion, representing diverse educational backgrounds. I selected this program for its comprehensive coverage of human and veterinary vaccinology, delivered by renowned experts from Oxford University, The Jenner Institute, and The Pirbright Institute. Notably, the course featured instructors who played pivotal roles in developing the COVID-19 (AstraZeneca & University of Oxford) and malaria (R21/Matrix-M vaccine, Serum Institute of India & University of Oxford) vaccines, which were examined as case studies. Additionally, the curriculum encompassed various other significant topics such as vaccine formulations, adjuvants for vaccines in clinical trials, and the innovation of multivalent vaccines for poultry viral diseases.
Over the course of five days, I gained insights into various aspects of vaccine research and development, spanning from inception to clinical studies. The remaining topics concerning vaccine manufacturing, quality control, and pertinent laws and regulations will be covered in the second part of this course, titled "Clinical Vaccine Development and Biomanufacturing," which I intend to enroll in future. However, for this article, I summarized what I learned into four key lessons as follows.
FIRST LESSON: COVID-19 Altered the Vaccine Development Landscape. Prior to COVID-19, the process of developing a vaccine typically spanned 5-10 years. However, the urgency of the pandemic compressed this timeline to approximately 350 days. Consequently, this event has fundamentally shifted the mindset of all stakeholders in vaccine development. In response to this paradigm shift, the Coalition for Epidemic Preparedness Innovations (CEPI) has implemented best practices aimed at further accelerating vaccine development, with a goal of achieving a 100-day timeframe. Hence, for any research group engaged in vaccine development, CEPI's aspiration of achieving a 100-day timeframe should serve as a guiding principle for future endeavors.
SECOND LESSON: Vaccinology Presents Unprecedented Financial Opportunities. As of 2023, the global population reached an estimated 8.1 billion people. However, the current annual global vaccine supply stands at only 500 million doses, with the majority of sales (80%) occurring in developed nations such as the USA, Japan, and European countries. Furthermore, the market size for vaccines has surged from $5 billion in 2000 to $20 billion in 2012, with projections indicating a value of $54 billion by 2024. This fully highlights a significant gap between supply and demand, considering both market size and global population and present a room for growth for vaccine developers. Additionally, approximately 23% of profits ($4.6 billion to $12.4 billion) were reinvested into research and development (R&D) by pharmaceutical companies. This presents funding opportunities for academics and universities to propose collaborations with vaccine developers in the field of vaccine development.
THIRD LESSON: Large Animals are Better Predictor for Human Immunogenicity Compared to Small Animals. Professor Jayne Hope (Roslin Institute, University of Edinburgh) shared this insight based on her experience studying NK receptor families across species and animal immune defense. Associate Professor Rachel Tanner (Department of Biology, University of Oxford) echoed a similar sentiment from her experience in developing tuberculosis (TB) vaccines. Rachel presented her immunological study data from mice and cows, then compared their results to human immunological studies. She concluded that the data from cows were more similar to human data than the data from the mice study.
FOURTH AND FINAL LESSON: Vaccine is a Multidisciplinary Field – So Network Effectively. Recently R21-Matrix-M (R21-MM) vaccine was the second malaria vaccine approved by World Health Organization (WHO). R21-MM vaccine was developed by many scientists from different part of the world as listed in Figure 1.
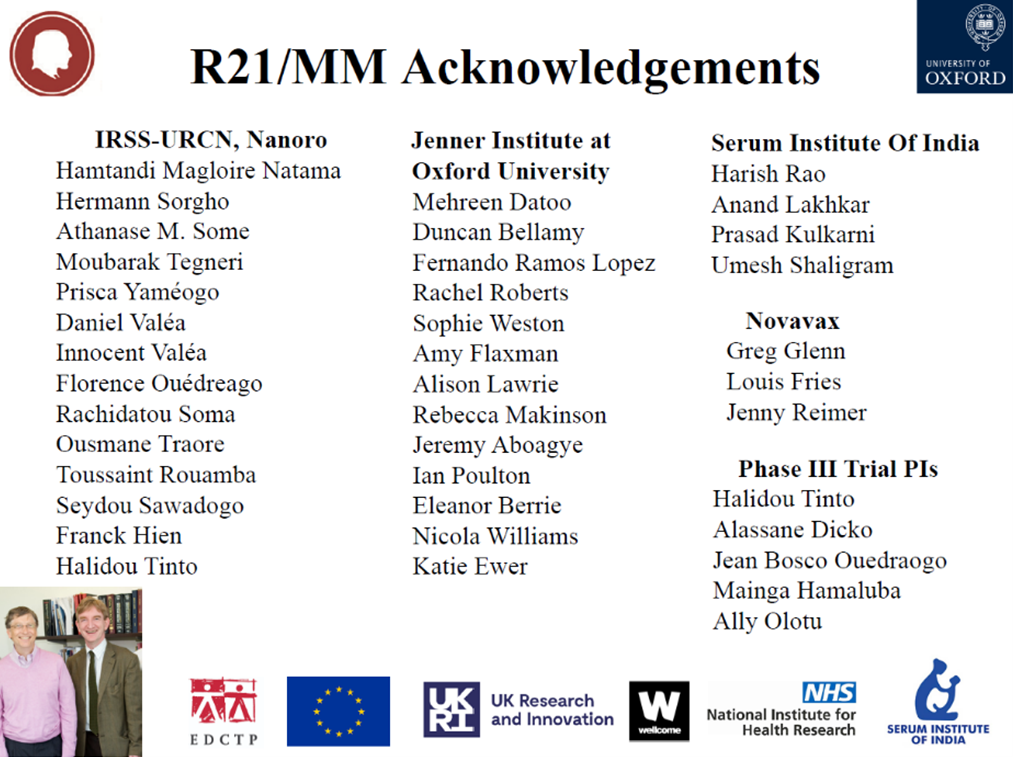
Figure 1: List of scientists and institutes that collaborated to produce the R21-MM malaria vaccine.
Networking allows for a better, faster, cheaper, easier to manufacture vaccine production by design through enabling of sharing of experience, data, cost, facilities, technologies and expertise. Networking also brings government agencies, industries, academia and philanthropist ore relevant funding bodies together on research and development of vaccines and related policy tools. Overall, effective networking will improve vaccine development from bench to bedside at lower cost.
In conclusion, I have benefited from attending this course. As such, I would like to express my heartfelt appreciation to the National Institute of Biotechnology Malaysia (NIBM) and the Malaysian government, specifically the Ministry of Science, Technology and Innovation, for graciously sponsoring my attendance in this course.
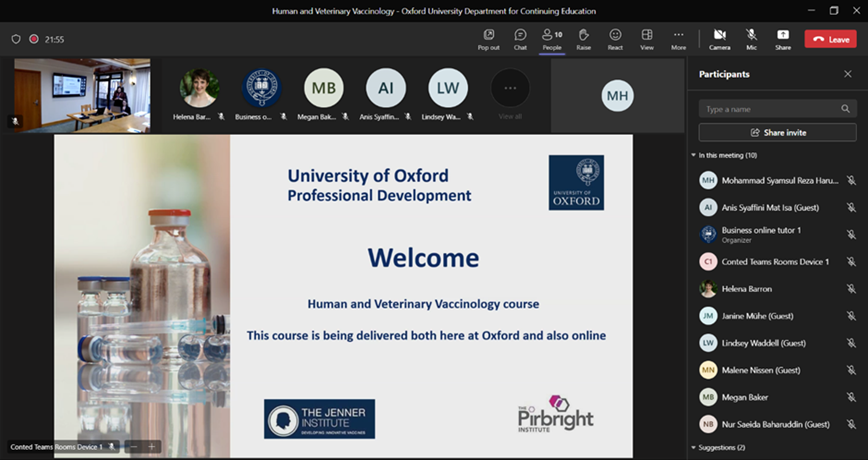
Figure 2: First day of as online course participant using Microsoft Teams platform.
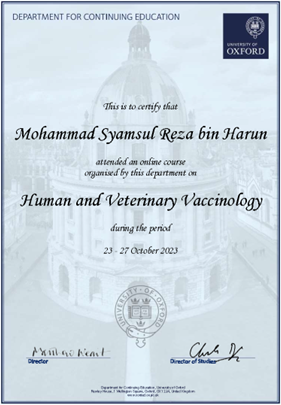
Figure 3: The digital certificate is provided upon the completion of the course.
Penulis Artikel:
Dr. Mohammad Syamsul Reza Harun
Afiliasi:
1. Jabatan Sains Bioperubatan, Institut Perubatan dan Pergigian Termaju, Universiti Sains Malaysia
2. Kumpulan penyelidikan ‘Emerging Infectious Disease (EID): Preparation for Disease X’
Bidang kepakaran:
Parasitologi, Bioinformatik, Virologi