These warning signs was translated by the Malaysian Patient Organisation for Primary Immunodeficiencies (MYPOPI). Consultation with Primary Immunodeficiency experts is strongly suggested.
Primary immunodeficiency diseases (PID) is a disease caused by defective immune system leading to increased susceptibility to infection and maybe fatal. It involves diverse phenotype which may include susceptibility to infections, allergy, immune dysregulations and auto-inflammation. With the advance of exome and genome sequencing, more than 500 identified genetic defect causing PID worldwide.
Each individual has his or her own blueprint, a map made up of millions of bits of information called genes. The gene-map of each individual is a unique mix of genes from the mother and father. This map instructs the body how to build and how to maintain itself. Sometimes there are malfunctions in this map. When it fails to produce a functioning immune system, the disease resulting is called a primary immune deficiency (PI). Sometimes there may be a history of such a malfunction in the family, but often there is not. It all depends upon how the genes of the parents have come together to make up the blueprint for a unique and distinct individual.
Looking at the local data, as of 2020, a prevalence of 0.37 per 100,000 people was reported from a systematic review of 34 publications. No further description on PID genotypes or survival outcome reported from this cohort. There is a major discrepancy compared to registry data reported from other countries in the world. We postulated the main reason of low PID cases in Malaysia is due to many patients were undiagnosed and undetected.
What are some types of PID?
1. Severe Combined Immunodeficiency (SCID)
SCID is a group of rare, life-threatening disorders caused by mutations in different genes involved in the development and function of infection-fighting T and B cells. Infants with SCID appear healthy at birth but are highly susceptible to severe infections.
2. Chronic granulomatous disease (CGD)
It is defined as an inherited phagocyte disorder causing defective superoxide generation and intracellular killing. Reduced or missing burst activity (nicotinamide dinucleotide phosphate (NADPH) oxidase complex) is observed in this inborn defect that usually manifests itself during the first two years of life. It can be inherited either by X-linked inheritance or autosomal recessive inheritance. Most patients with CGD develop failure to thrive, severe bacterial adenitis, abscesses, osteomyelitis or hyperinflammatory manifestations.
3. Common Variable Immunodeficiency (CVID)
This PI is marked by lower blood levels of two immune-globulins, IgG and IgA, and in about half the cases, of a third immune-globulin, IgM. People with CVID do not make sufficient or effective antibodies to fight bacterial and viral infections. The most common symptoms initially are recurrent and difficult to clear infections of ear, nose, sinuses, bronchi and lungs. CVID affects males and females in equal number. Some display symptoms early in life, and some not until their twenties or later.
4. X-Linked Agammaglobulinemia
XLA is a PI affecting males, caused by an inability to produce B cells or immunoglobulins (antibodies), which are made by B cells. People with XLA develop frequent infections of the ears, throat, lungs, and sinuses.
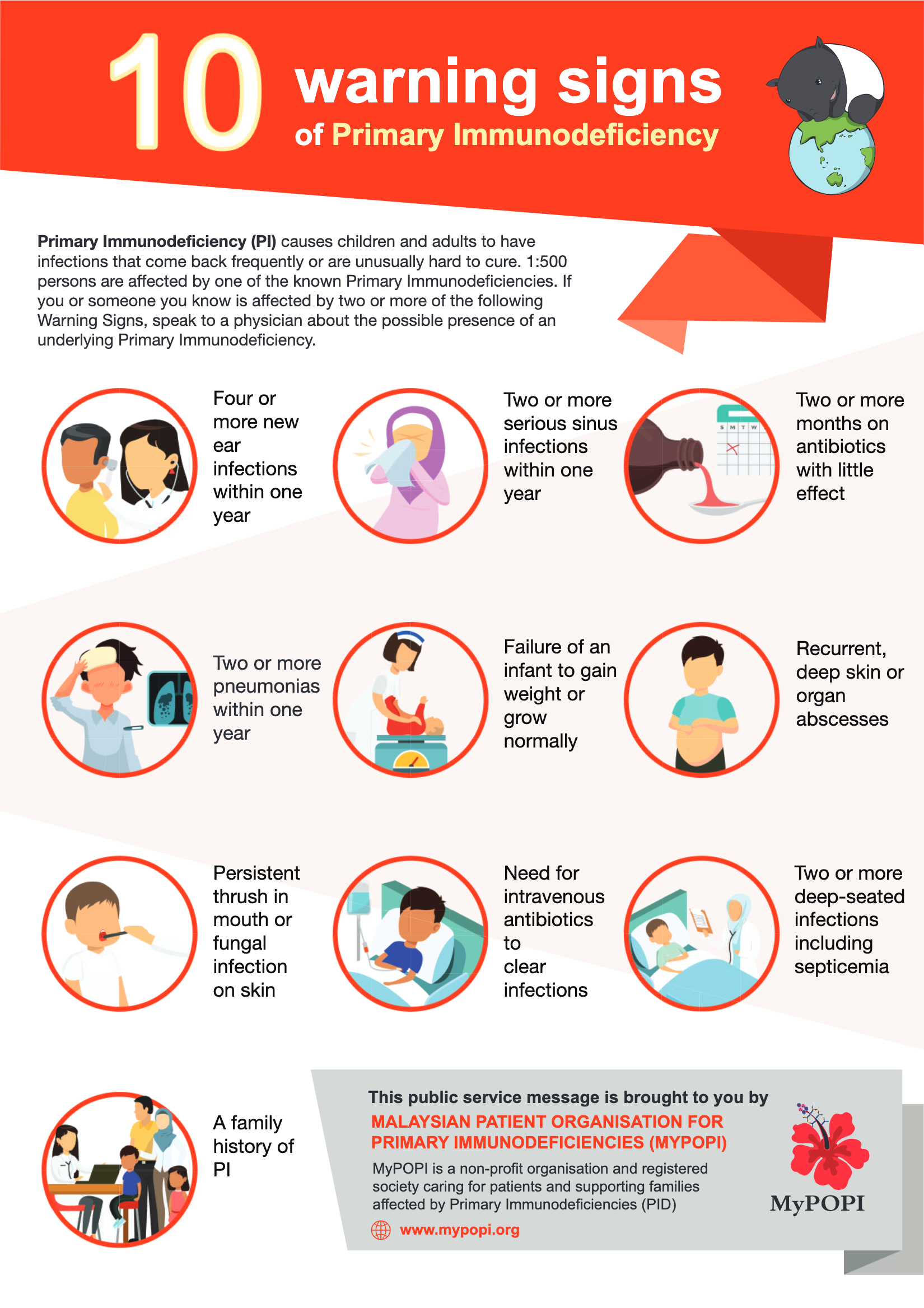
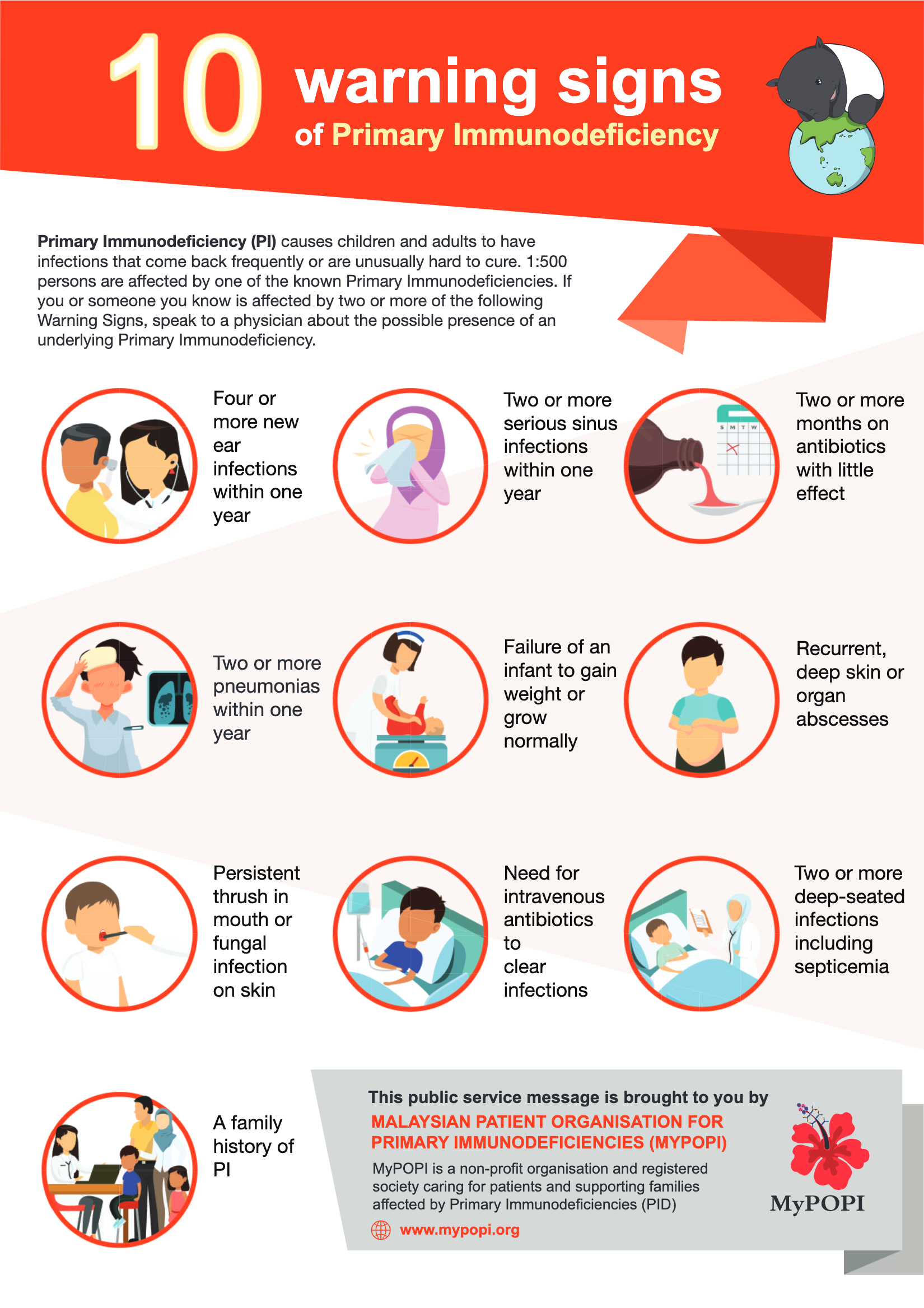
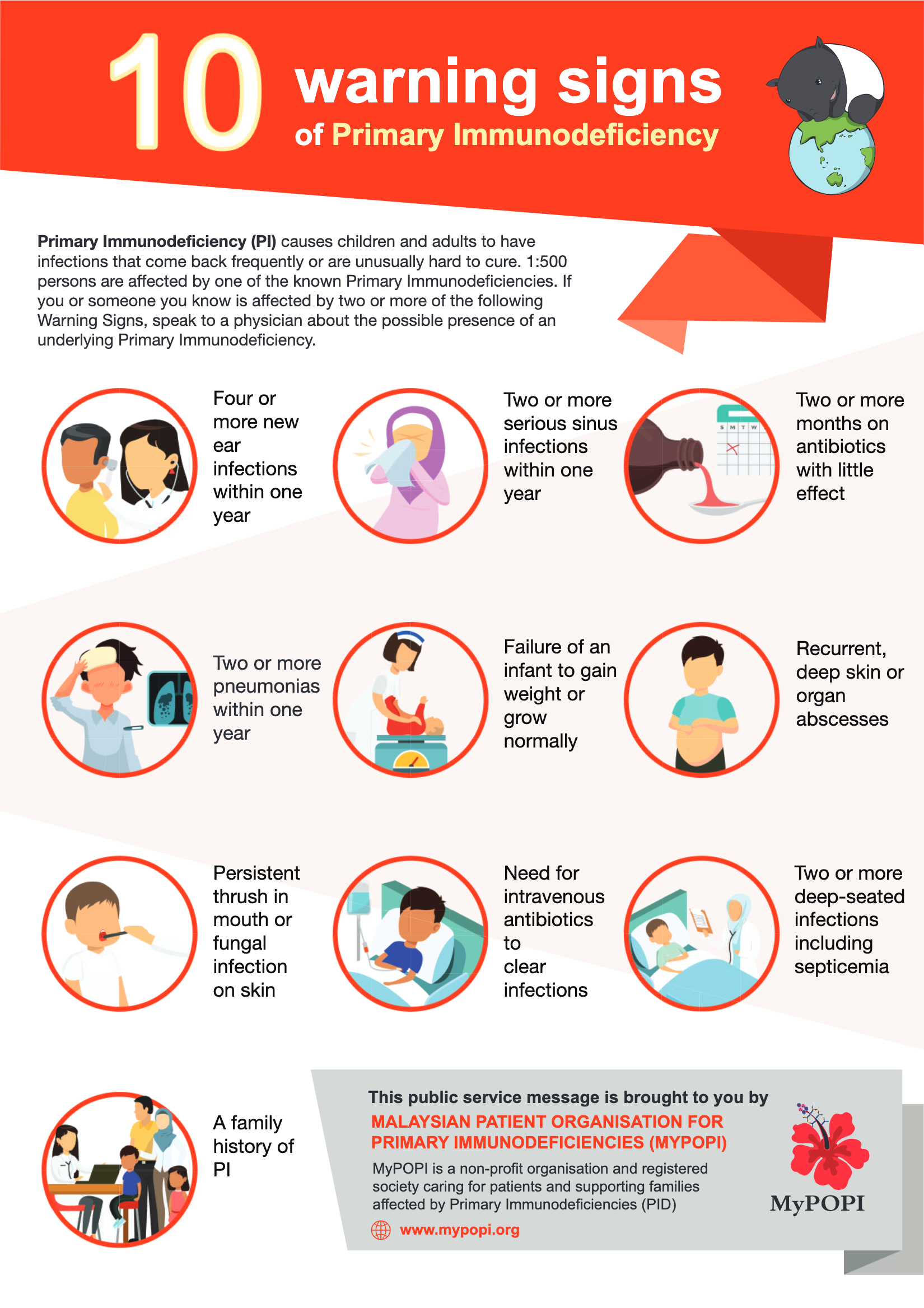
10 Warning Signs of Primary Immunodeficiency
If your child has two or more of these signs, ask your doctor about Primary Immunodeficiency. It could save your child’s life.
How is PID diagnosed and treated?
1. Laboratory Testing
Laboratory studies are necessary to determine the presence of a PID. This is usually prompted by an individual experiencing some clinical problems, particularly recurrent and/or chronic infections. The patient’s medical history and physical exam direct the appropriate choice of laboratory tests.
a) Primary Immunodeficiency Diseases Unit at USM Medical Centre Bertam (PPUSMB)
The Primary Immunodeficiency Disease Unit caters for clinical referrals from Northern and Eastern Malaysia (Kelantan and Terengganu). The centre comprises a diagnostic lab which does some immunological and allergy tests.
The team is headed by Dr Intan Juliana Abd Hamid, a consultant Paediatric Immunology & Allergy, supported by scientists working on functional and molecular/genetic aspects of PID and staff nurses. This centre is also listed on Jeffrey Modell Foundation website.
There are other specialised centres for PID Care with clinical immunologists in our country, like Pantai Hospital, Kuala Lumpur (Dr Amir Hamzah), Hospital Pengajar UPM (Assoc Prof Dr Intan Hakimah, Dr Azri), UKM Specialist Children's Hospital (Assoc Prof Dr Adli Ali) and Hospital Kuala Lumpur (Dr Sangeetha, Dr Marina) / Institut Medical Research (HKL/IMR).
2. The need for Newborn Screening in Malaysia
Severe Combined Immune Deficiency (SCID) leads to life-threatening infections unless the immune system can be restored through a bone marrow transplant, enzyme replacement or gene therapy. Infants with SCID who lack a family history have been diagnosed in the past only after developing serious infections. Early identification of SCID through screening of all newborns can make possible life-saving intervention before infections occur.
Looking back in current local situation, there is no available report or published evidence of newborn screening for PID patients in Malaysia to date. The dearth of local evidence is striking. It is timely to further the research work in characterization of thymic output in Malaysian PID cohort prior to therapeutic intervention.
3. How PID is treated?
A patient with a PI will be treated for any current infection with specific antibiotics, anti-viral or antifungal medications. In some PIs, to prevent permanent organ damage from recurrent infections, low or moderate doses of antibiotics may be recommended.
Around 30% of PID cases consist of antibody-deficiency types, like X-linked agammaglobulinaemia. These patients who although they lack immunoglobulin and so they are prone to infections, there is such a thing as commercially prepared immunoglobulin.
Patients can lead a relatively normal life with intravenous immunoglobulin, (IVIg). IVIg usually is scheduled every three to four weeks, and once started, treatment is usually lifelong. In Malaysia, IVIg is subsidised in public hospitals for patients of all ages who need it to stay alive.
Another type of PID involves defects in the innate immune system, which covers the cells and mechanisms that defend the body in a non-specific manner. In these most severe cases, where the immune system is completely non-functional (SCID), or chronic granulomatous disease (CGD), where there is a defect in the patient’s neutrophils, a bone marrow transplant may be required. Currently, the transplant is only available in a handful of hospitals in Malaysia.
What is the future of PID in Malaysia?
Among the challenges PID patients face is the lack of awareness about the condition. One of the solutions to this problem is to have more clinical immunologists. Ideally, there should be one in every regional hospital, so that other doctors can call them for consultation.
Finally, in conjunction with the ongoing Primary Immunodeficiency Disease Awareness Week Programme 2024, come and support us to celebrating life and what keeps the PID community moving forward. There are health and research exhibitions, webinars on introduction and current advances in managing the disease and PID book launch. This event was made possible through collaboration between PPUSMB, IPPT USM and Immunocare Sdn Bhd, with MPA (Penang state branch) and MyPOPI.