Introduction
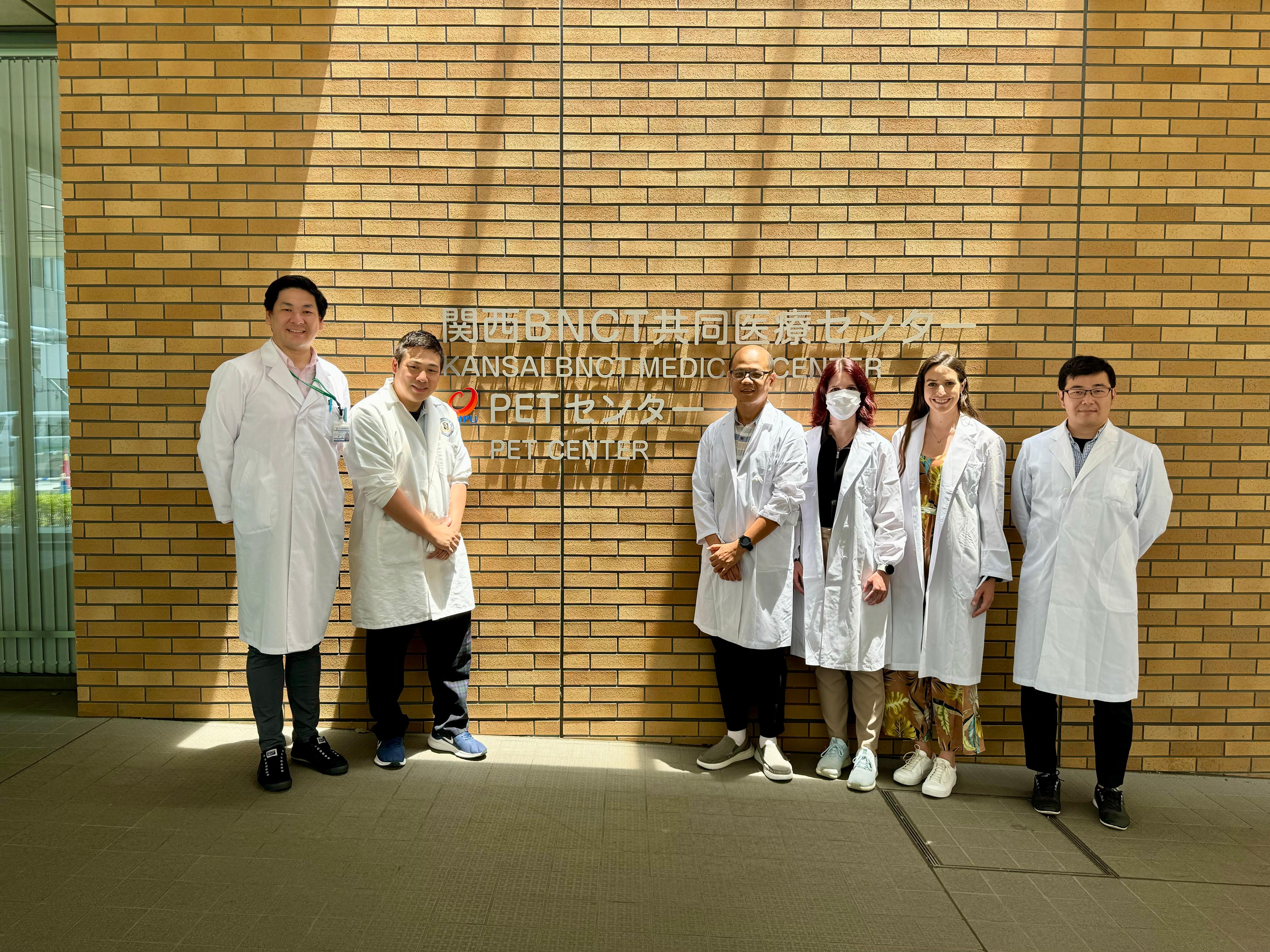
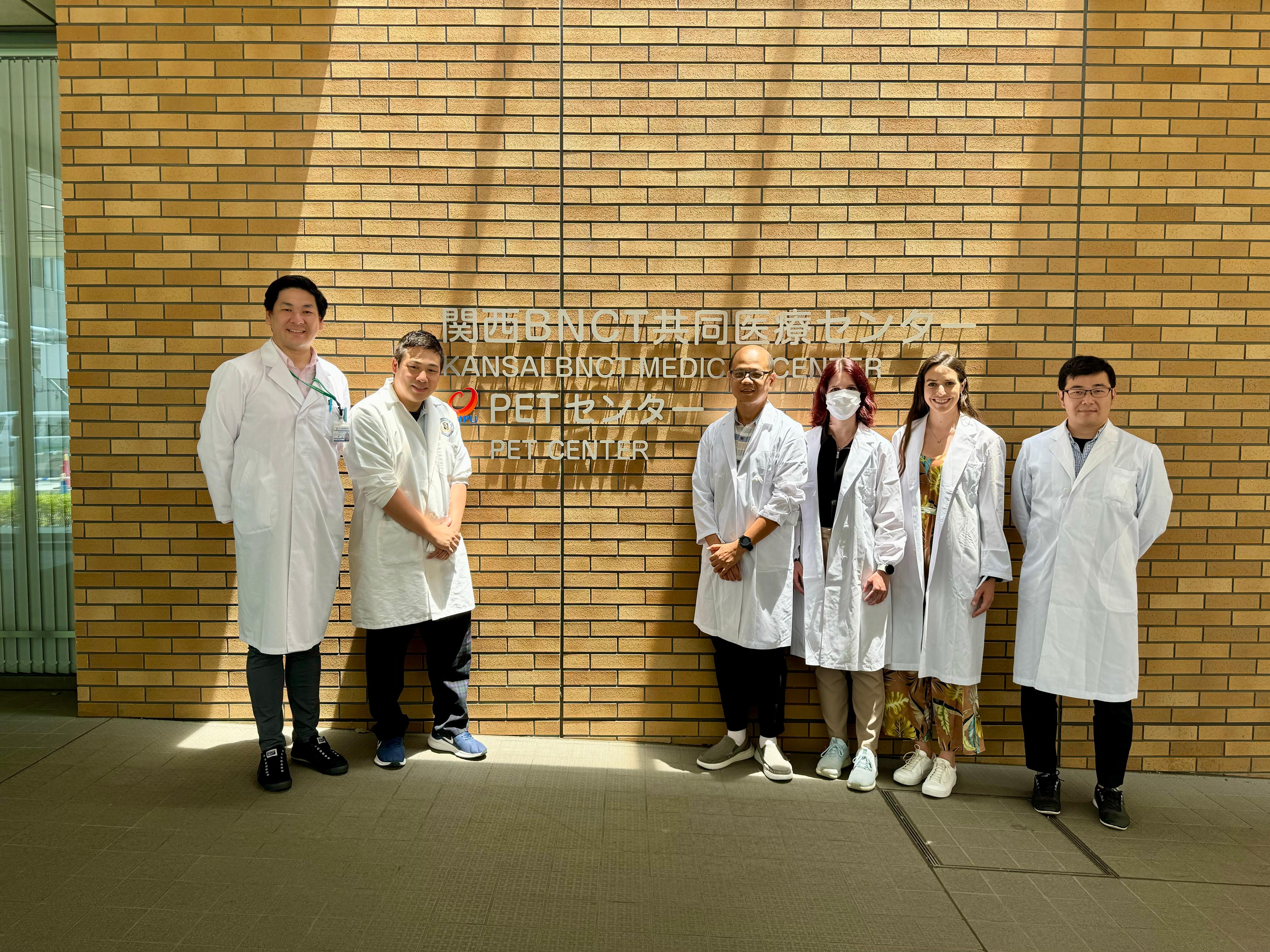
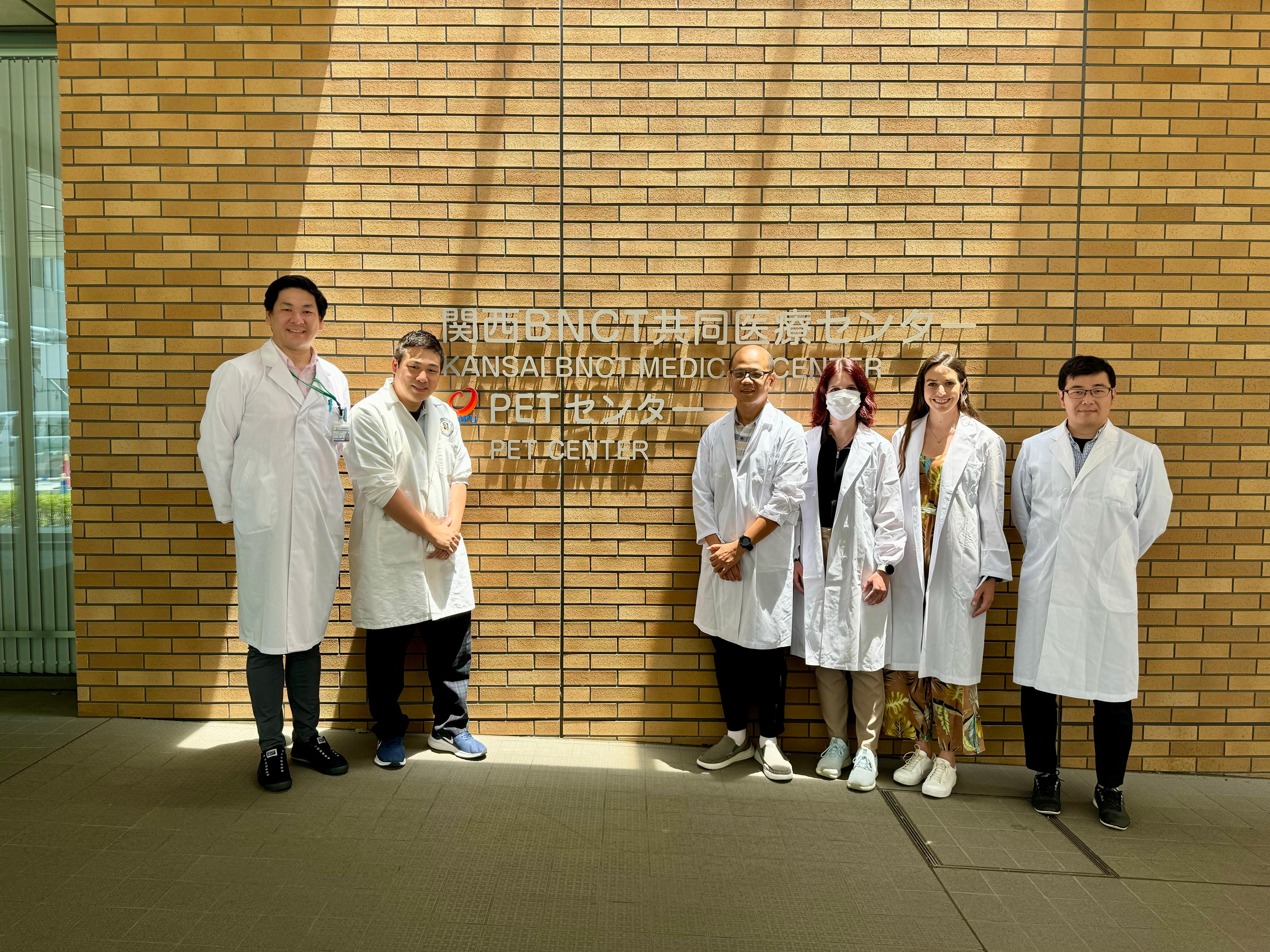
Under the collaboration between the Advanced Medical & Dental Institute, Universiti Sains Malaysia, and the Osaka University Graduate School of Medicine, Japan, the author visited the Kansai Boron Neutron Capture Therapy (BNCT) Medical Center and the Institute of Integrated Radiation Research at Kyoto University (KURNS) in the summer of 2024. The author would like to share the latest techniques in precision cancer therapy developed at KURNS, Japan.
Photo By Kansai BNCT Medical Center
Figure 1: Visit to the Kansai BNCT Medical Center on June 19, 2024 (left
to right: Kansai BNCT Medical Center Physicist Associate Prof.Dr.
Naonori, Associate Prof. Dr. Kazumasa from Osaka University Graduate
School of Medicine, the author from Advanced Medical and Dental
Institute, Malaysia, Anna from Budapest Semmelweis University, Dr. Aliz
from Budapest National Institute of Oncology and, Associate Prof. Dr.
Sakata from Osaka University Graduate School of Medicine)
Boron Neutron Capture Therapy (BNCT) was first proposed by American physicist Gordon Locher in 1936, using neutron capture reactions to destroy cancerous tumors, four years after Sir James Chadwick discovered the neutron in 1932. Japan has made great progress in the development of BNCT, leading to significant advancements in the field today. BNCT, which uses a boron target bombarded by a neutron beam, kills cancer cells more precisely than conventional radiotherapy. This advanced technique provides another hope for end-stage cancer patients, especially those suffering from head and neck cancer.
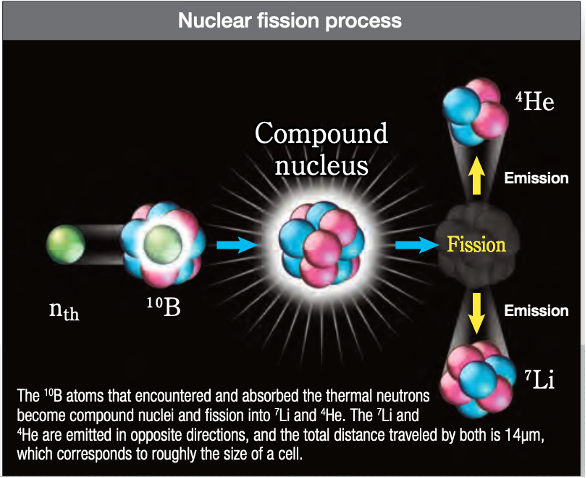
The treatment of BNCT is positioned between chemotherapy and external particle therapy. It uses the nuclear reaction between boron and neutrons to selectively destroy cancer cells, providing safe and precise treatment modalities for cancer patients. Pre-administered boron compounds containing the stable isotope boron-10 are given to the patient and are selectively absorbed by the cancer cells. The cancer cells are then exposed to thermal neutron beams, causing a nuclear reaction with boron-10 as shown in the equation below. This reaction generates lithium nuclides and short-range alpha particles, with a range almost similar to the cell diameter, which destroy the cancerous cells from the inside while minimizing damage to surrounding normal tissues. [1-3]
10B5 + 1N0 -> [11B5]* -> 4He2 (aplha)+7Li3 + gamma equation (1)
Photo By Pioneered by Japanese Brainpower
Figure 2: Boron neutron capture reaction generates lithium nuclides and
short-range alpha particles (Source: Pioneered by Japanese Brainpower:
New Horizons in Cancer Treatment - Boron Neutron Capture Therapy [3])
Neutron Source and Clinical ResearchThere are two methods for producing a neutron source for BNCT: reactor-based and accelerator-based. Accelerator-based sources have many advantages over reactor-based sources, such as being easier to handle, safer, having lower set-up costs, and being smaller in size, which allows for installation within hospitals. Additionally, the installation and maintenance of accelerators are easier than those of reactors, the neutron flux produced by the accelerator is much higher than that produced by the reactor because the efficacy of BNCT depends heavily on the ability to deliver sufficient boron to the cancer cells and tissues selectively [2-3]. Technological improvements in neutron sources and boron delivery are pivotal. The shift from reactor-based to accelerator-based neutron sources is a significant trend. Accelerator-based neutron sources have become more feasible due to advances in accelerator technology, offering a safer and more reliable alternative to nuclear reactors.
The Institute of Integrated Radiation Research at Kyoto University (KURNS) developed the world's first accelerator-based BNCT in 2009, in collaboration with Sumitomo Heavy Industries. KURNS had been conducting clinical research on BNCT using a research reactor since 1990. After successfully developing an accelerator neutron source using a cyclotron, the clinical study using this reactor-based system was stopped in the year 2018. Other than KURNS, reactor-based BNCT is also performed at the National Atomic Energy Commission in Argentina, the National Tsing Hua University in Taiwan [4]. Shifting from reactor-based BNCT to accelerator-based BNCT is highly recommended and promoted due to its many advantages. At present, BNCT clinical studies are also being carried out in several countries, including the United States, the Netherlands, Germany, Italy, the Czech Republic, and Sweden. [2].
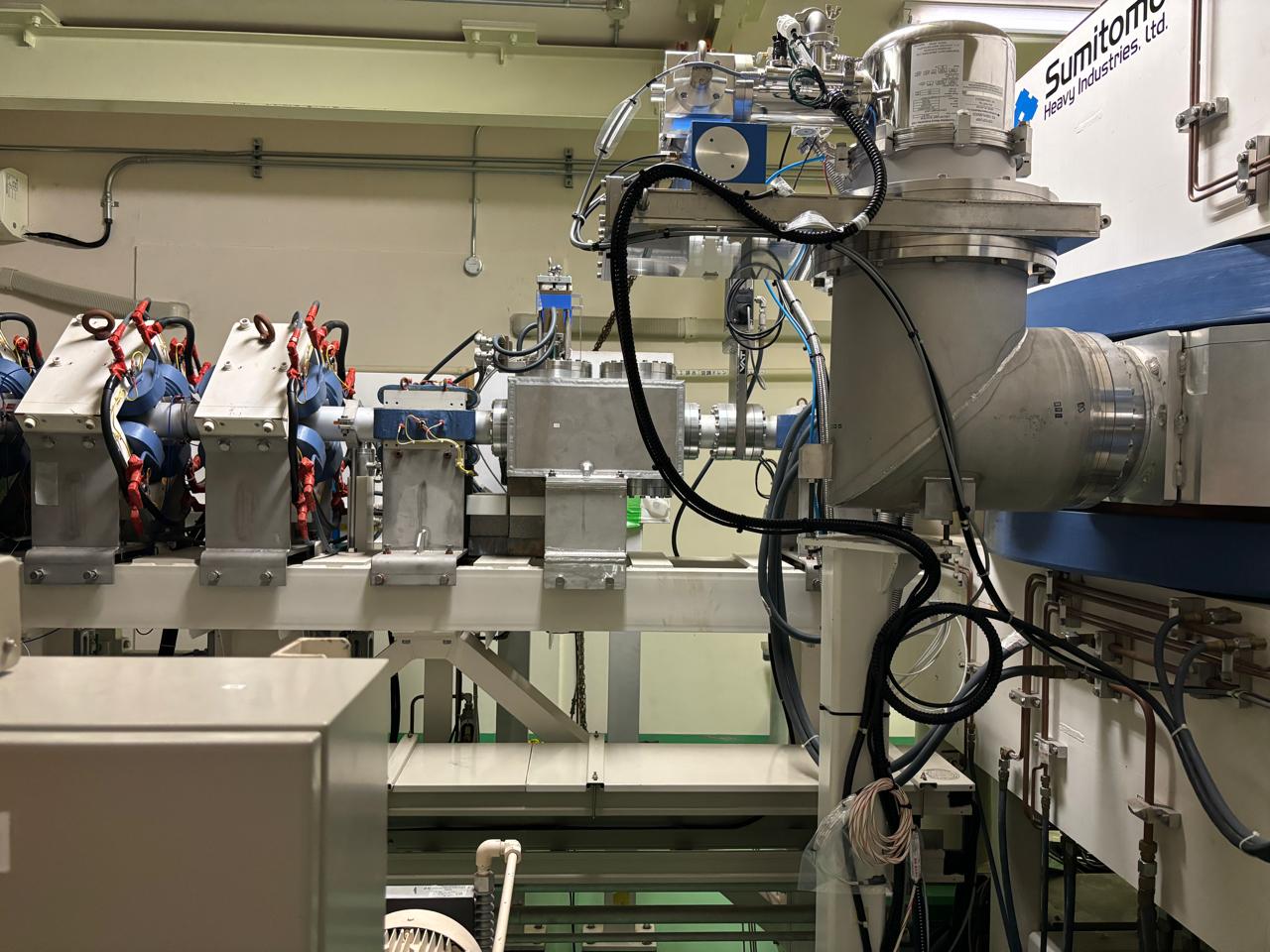
Photo By Ying Chee Keat
Figure 3 (a): Accelerator based of Neutron Source located in the KURNS,
Osaka, Japan. The pictures were taken by the author visited the
facilities on July 12, 2024.
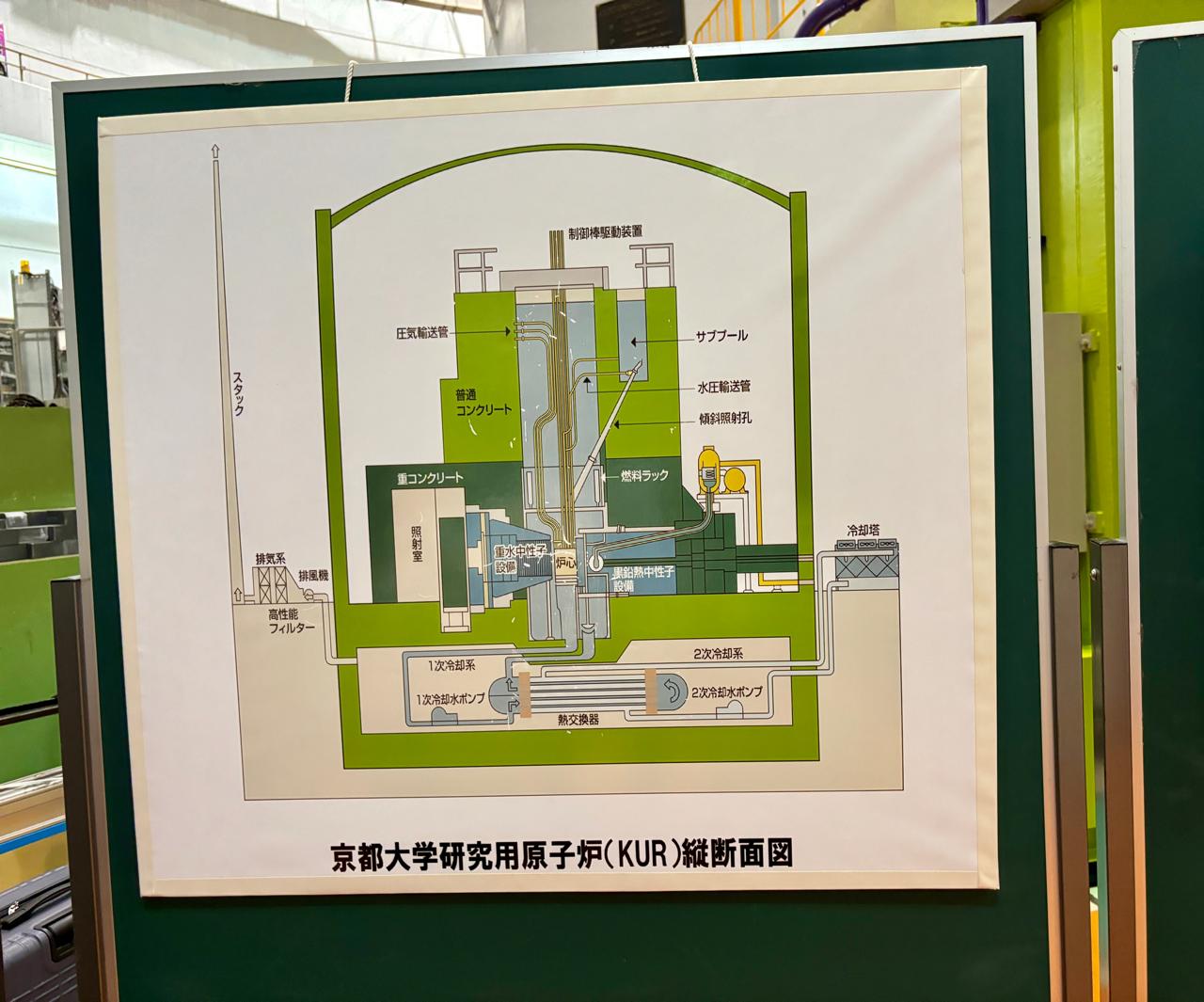
Photo By Ying Chee Keat
Figure 3 (b): Reactor based of Neutron Source located in the KURNS, Osaka, Japan.
Kansai BNCT Medical CenterIn 2018, the Kansai BNCT Medical Center, located in Osaka, Japan was completed. In 2020, Japan became the first country to approve BNCT for unresectable advanced or recurrent head and neck tumours, with coverage provided by the national insurance program, requiring patients to pay only 30% of the treatment cost. Clinical trials are ongoing for relapsed brain tumours and head and neck cancer in Kansai BNCT Medical Center. Researchers from Japan and many other countries are visiting the Kansai BNCT Medical Center for various types of research.
The author visited the Kansai BNCT Medical Center for two days in 2024 to observe the treatment operations under the Osaka University International Certificate Program (OUICP). During the first day, the author observed the entire treatment process for a patient with a recurrent neck tumour. BNCT requires only a single fraction, and the radiation time is approximately 40 to 60 minutes. The total treatment time can extend to two hours or more including the time needed for patient positioning and preparing. The patient must maintain their position during the beam time, which can be somewhat uncomfortable for the patient compared to conventional radiation therapy. However, the advantage of BNCT is that it only requires a single fraction, whereas conventional radiation therapy requires multiple fractions.
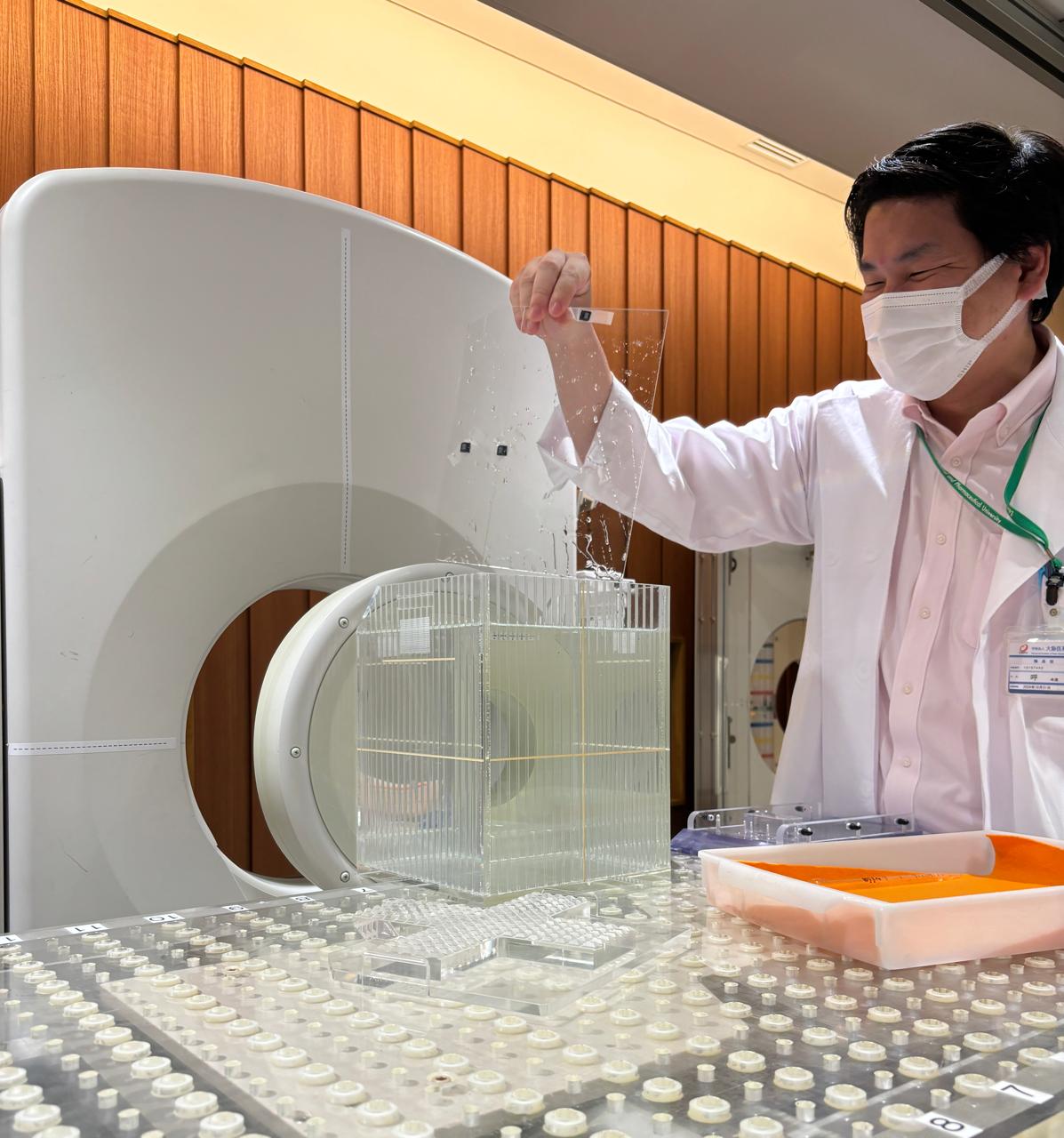
During the second visit, the author observed the weekly quality assurance (QA) of the BNCT irradiation system. Similar to conventional radiotherapy, the BNCT irradiation system must conduct daily, weekly, monthly, and yearly quality assurance to ensure safety, accuracy, and overall quality management. During the weekly QA, physicists perform dose measurements using gold wire. The gold wire is cut into square shapes and attached at three positions on the Perspex inside a water phantom. After the gold wire is irradiated by neutrons, the induced radioactivity is measured. Besides the gold wire, the physicists also demonstrated other types of dosimeters for different purposes, such as semiconductor detectors and Thermoluminescent Dosimeter (TLD) detectors. In the same visit, the author also observed the setup for patient positioning, mask making, CT simulation for target localisation, and treatment planning for the upcoming treatment. These procedures are also similar to those in conventional radiotherapy.
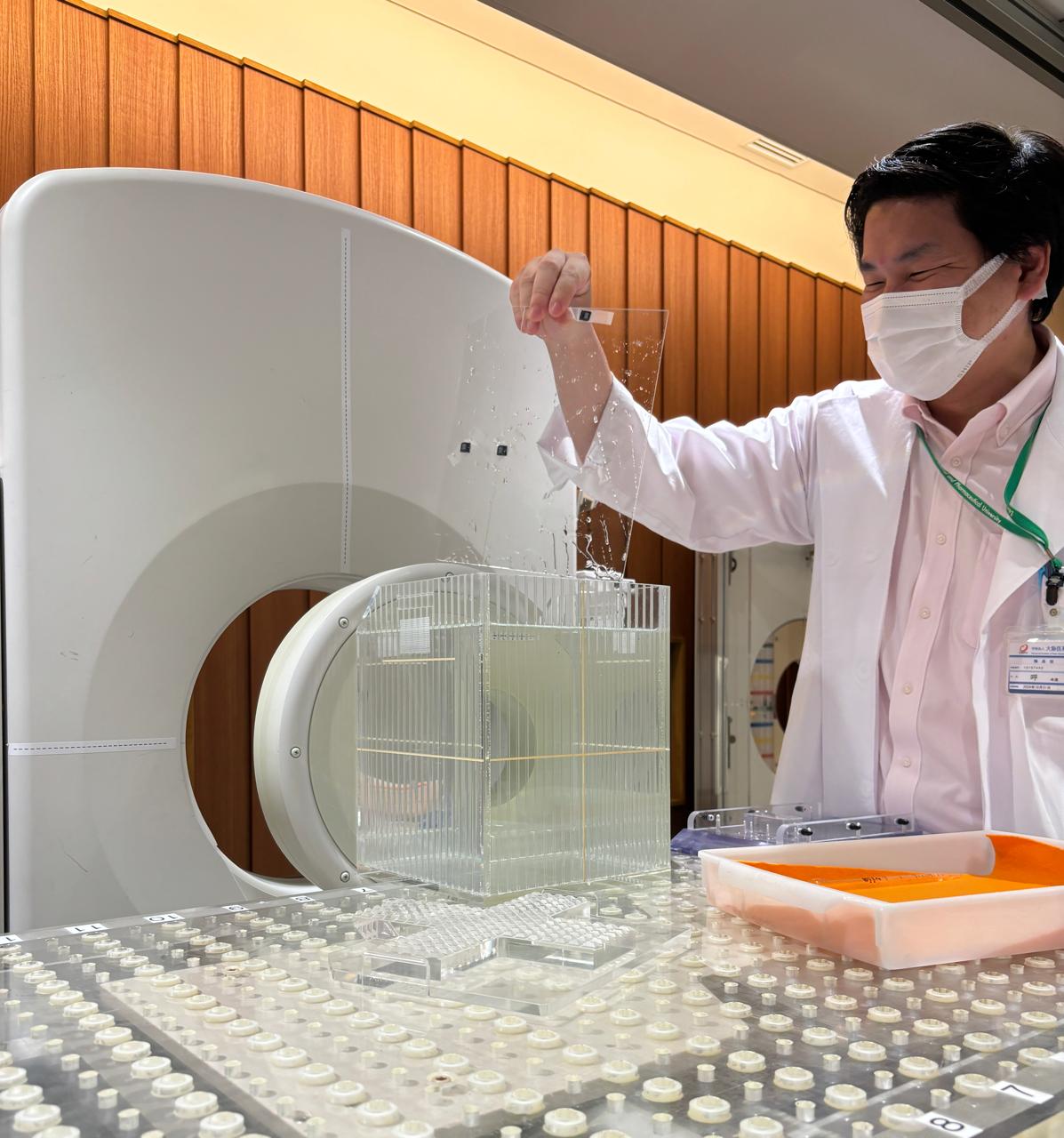
Photo By Ying Chee Keat
Figure 4: Physicist performing quality assurance of the BNCT irradiation
system, the pictures were taken by the author visited the Kansai BNCT
Medical Center on July 11, 2024
Conclusion
BNCT is a treatment method that combines radiation, nuclear physics, chemistry, biology, and medicine. It represents an emerging targeted therapy with promising results and acceptable toxicity in clinical studies. BNCT has many advantages, such as substantially less damage to normal tissues, applicability for recurrent cancer after radiotherapy, and a short treatment period with only a single fraction. At present, the BNCT treatment modality is used to treat malignant glioma and recurrent head and neck tumors in patients who have not responded to conventional treatment [5-8]. This treatment modality is also being investigated for other target cancers, such as lung cancer, liver cancer, breast cancer, metastatic disease, and more. More clinical trials are needed to evaluate the safety and efficacy of BNCT.
References
1. Malouff TD, Seneviratne DS, Ebner DK, Stross WC, Waddle MR, Trifiletti DM, Krishnan S. Boron Neutron Capture Therapy: A Review of Clinical Applications. Front Oncol. 2021 Feb 26;11:601820. doi: 10.3389/fonc.2021.601820. PMID: 33718149; PMCID: PMC7952987.
2. He, H., Li, J., Jiang, P. et al. The basis and advances in clinical application of boron neutron capture therapy. Radiat Oncol 16, 216 (2021). https://doi.org/10.1186/s13014-021-01939-7
3. Pioneered by Japanese Brainpower: New Horizons in Cancer Treatment (Boron Neutron Capture Therapy)
4. Sakurai, Y., Tanaka, H., Takata, T. et al. Advances in boron neutron capture therapy (BNCT) at kyoto university - From reactor-based BNCT to accelerator-based BNCT. Journal of the Korean Physical Society 67, 76–81 (2015). https://doi.org/10.3938/jkps.67.76
5. Kankaanranta L, Saarilahti K, Makitie A, et al. Boron neutron capture therapy (bnct) followed by intensity modulated chemoradiotherapy as primary treatment of large head and neck cancer with intracranial involvement. Radiother Oncol. 2011;99(1):98–9.
6. Kankaanranta L, Seppala T, Koivunoro H, et al. Boron neutron capture therapy in the treatment of locally recurred head-and-neck cancer: final analysis of a phase I/II trial. Int J Radiat Oncol Biol Phys. 2012;82(1):e67-75.
7. Kimura Y, Ariyoshi Y, Shimahara M, et al. Boron neutron capture therapy for recurrent oral cancer and metastasis of cervical lymph node. Appl Radiat Isot. 2009;67(7–8 Suppl):S47–9
8. Xu D, Zhang YC, Zhou QY, et al. Boron neutron capture therapy of cancers: principles and recent research progress. Chin J Radiol Med Prot. 2021;41(1):74–7.