
Figure 2: Similar name but different date of birth (DOB)


Blood
transfusions are lifesaving medical procedures commonly used to replace blood lost
due to surgery, injury, or illness. Although it is routine in medical settings,
many people may feel anxious or uncertain about what happens during the
process. In Malaysia, it is estimated about 2,000 blood bags are transfused
daily.
Patients
may receive different blood products depending on their specific medical needs.
The most common blood product transfused is red blood cell (RBC), which is used
to treat severe anaemia or massive bleeding. Meanwhile, platelet product is
used to treat individuals with bleeding issue due to platelet problem, while
plasma is usually administered to individual with blood clotting disorder.
The blood transfusion process can take place in a daycare or inpatient setting. In the daycare setting, the recipients usually have underlying chronic blood disorders that required regular blood transfusions, sometimes on a monthly basis, and possibly for life, as in the case of patients with thalassaemia major. These patients are generally stable and can return home after completing their transfusions. In the inpatient setting, transfusions are performed for hospitalised patients. Overview of the blood transfusion process is shown in Figure 1.
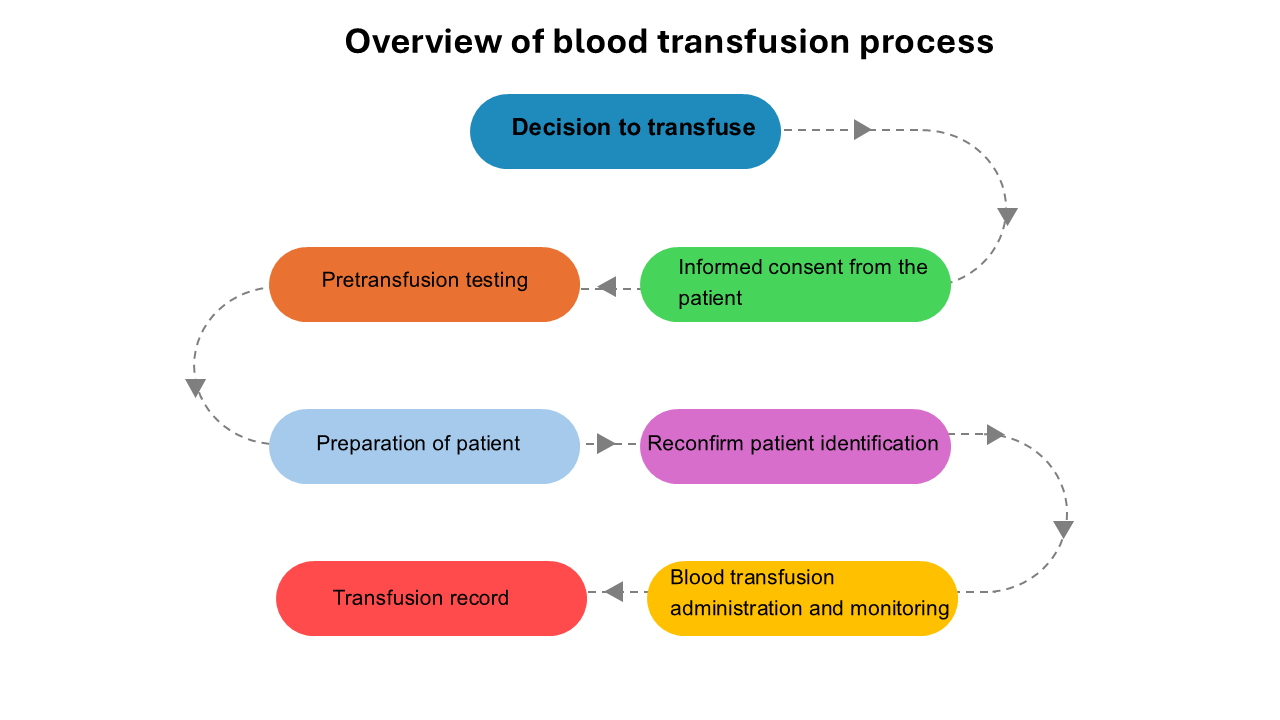
Photo By Siti Salmah binti Noordin
Figure 1: Overview of blood transfusion process
Before the Transfusion:
Consent and Pre-Transfusion Testing
Prior
to any blood transfusion, informed consent will be obtained from the patient by
the doctor in charge. During this process, the doctor will explain the
indications, risks, and potential complications related to the blood
transfusion. The patients must sign the informed consent form to indicate their
agreement for blood transfusion.
Once the informed consent is obtained, a blood sample will be drawn from the patient. In a fully conscious patient, the phlebotomist will confirm the patient's identity by asking them to state their full name and identification card number before labelling the blood sample tube. Therefore, it is essential for the patient to clearly state their full name and identification number and address any potential issues with name spelling (Figure 2).

Photo By https://www.utmb.edu/health-resource-center/two-forms-of-identification
Figure 2: Similar name but different date of birth (DOB)
The
blood sample will be sent to the blood bank laboratory for pre-transfusion
testing. The tests include are the determination of the patient's ABO and RhD
blood group - whether A, B, AB, or O, and RhD positive or RhD negative. In
addition to ABO and RhD blood grouping, if the patient requires an RBC
transfusion, the sample will also be tested for the presence of any unexpected
RBC antibodies (antibody screening) and crossmatched with the donor's blood.
Crossmatching is important to determine the compatibility between the patient’s
and donor’s blood. However, for platelet and plasma transfusions, antibody
screening and crossmatching are usually not performed.
Following
the pre-transfusion testing, the requested blood product will be issued to the
ward or to the inpatient staff.
Before transfusion:
Intravenous Line and Patient Identifications
A suitable intravenous (IV) line will be inserted into the patient before the blood product administration. In addition, the doctor will verify the blood bag and will reconfirm the patient's identity to ensure that the correct blood product is transfused to the correct patient. This identification check is typically performed by two healthcare personnel, such as a doctor and a staff nurse.
During Blood Transfusion: What Happens When You Receive Blood
Blood transfusion administration takes approximately 1 to 4 hours, depending on the volume and types of the blood products. Throughout the procedure, the patient's vital signs will be monitored, and any clinical signs of adverse transfusion reactions will be assessed (Figure 3).

Photo By Image generated by Bing Ai
Figure 3: Blood administration
Symptoms of adverse transfusion reactions may include itchiness, rashes, chills, fever, nausea, vomiting, or difficulty in breathing. These reactions could be caused by allergens or proteins in the blood products that may provoke an allergic reaction, passively transfused cytokines in the blood bag that may cause febrile non-haemolytic transfusion reaction, or by the presence of RBC antibodies, thay may cause haemolytic transfusion reaction. If any signs or symptoms occur, the transfusion will be stopped immediately, and appropriate treatment will be administered.
After the Transfusion: Recovery and What to Expect
After the
blood transfusions, the patient will be monitored for a period of time to
ensure they do not develop any signs and symptoms of transfusion reactions. In
addition to acute reactions, delayed transfusion reactions may also occur, such
as delayed haemolytic transfusion reaction (DHTR), which is due to the presence
of RBC antibodies that may not have been detectable during the pre-transfusion
testing. However, DHTR is rare. Symptoms of DHTR may include yellowish skin
discolouration, a drop in haemoglobin levels, muscle or joint pain, and fever
Typically, a single unit of RBC transfusion will increase the patient's haemoglobin level by about 1 g/dL, with anaemia symptoms improving within 24 hours post-transfusion. For platelet transfusion, a single unit of random platelet transfusion will increase the patient's platelet count by 5 to 10 x 109/L. For plasma transfusion, an improvement in clotting tests is usually observed, with clotting factors may increasing by approximately 30%.
While
blood transfusions are lifesaving procedures, it is essential to establish
appropriate transfusion indications and adhere to safety protocols to minimise
the risk of errors or adverse events, ensuring the best possible care for the patient.
References: