What Are Platelets?
Platelet is the smallest blood cell in our body, typically measuring 2-3 µm in diameter, which is about one fourth the size of red blood cells (RBC). Platelets are derived from megakaryocytes, which are produced in the bone marrow. Their production is regulated by thrombopoietin, a glycoprotein hormone predominantly produced by the liver (95%), as well as the kidney and bone marrow. An estimated 1011 platelets are produced daily and released into the bloodstream, with a lifespan of 8 to 10 days. The typical range of circulating platelets in adults is between 150 × 109/L and 450 × 109/L. Platelets play a crucial role in primary hemostasis after exposure to the subendothelial extracellular matrix, particularly collagen, following vessel wall damage. Once activated, platelets secrete mediators that facilitate platelet aggregation and the coagulation cascade.
Preparation of Platelet Products
Platelet concentrates can be prepared from whole blood or apheresis collection.
1. Whole blood-derived platelets (referred to as random platelet concentrates):
• One unit typically contains > 60 x 109 platelets, with a volume of approximately 50–70 mL.
• One unit of random platelet concentrates can increase the platelet count by 5–10 x 109/L in a 70 kg adult.
• An adult therapeutic dose typically requires 4 to 6 units of random platelet concentrate.
2. Apheresis platelets (plateletpheresis):
• One unit of apheresis platelets contains 200 x 109 platelets and can increase the platelet count by 20–40 x 109/L in a 70 kg adult.
• One unit of plateletpheresis is sufficient to provide one adult therapeutic dose.
• Plateletpheresis is generally preferred when there is a need to limit exposure to multiple donors, such as in immunosuppressed patients or those with a history of allergic transfusion reactions.
Platelet Storage Requirements
Platelet concentrates must be stored at room temperature (20–24°C) in a platelet agitator to allow oxygenation and prevent platelet activation and clumping before transfusion to a patient. They should not be refrigerated or placed on ice to maintain their hemostatic function. As a result, platelet products have a higher risk of bacterial contamination compared to other blood components. The expiry date for platelet components is only 5 days after collection, often leading to issues with platelet shortages.
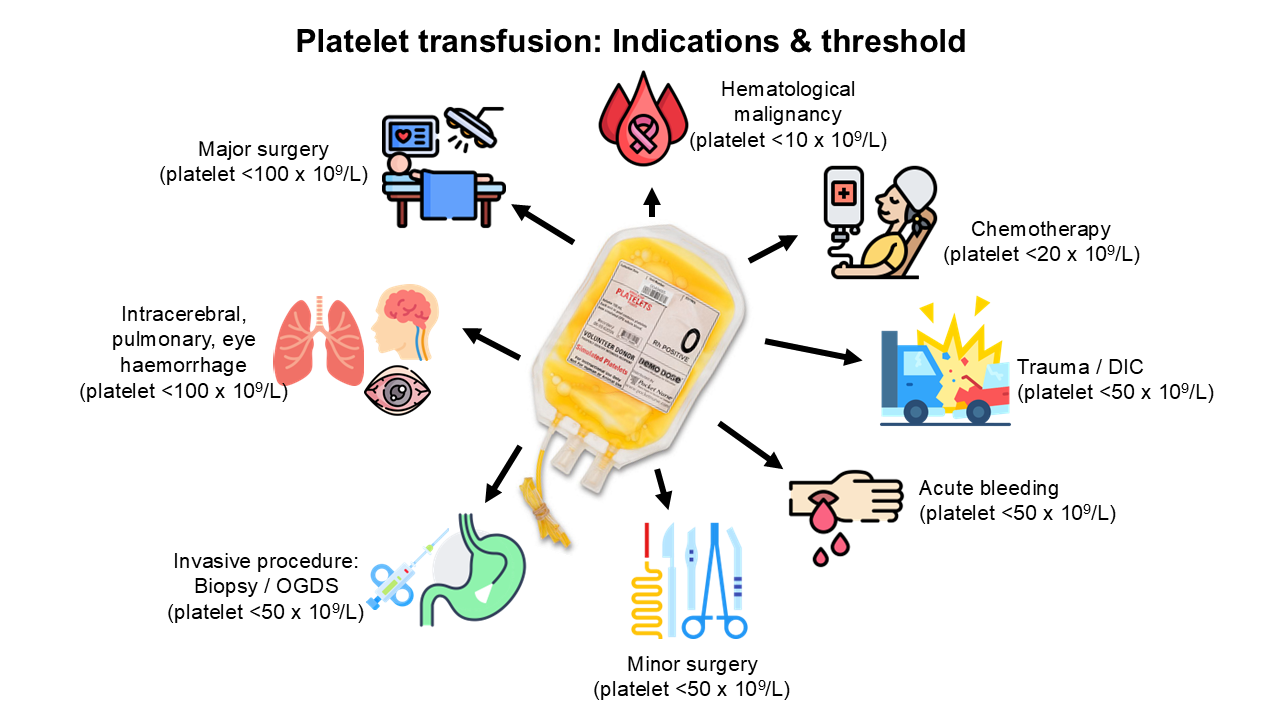
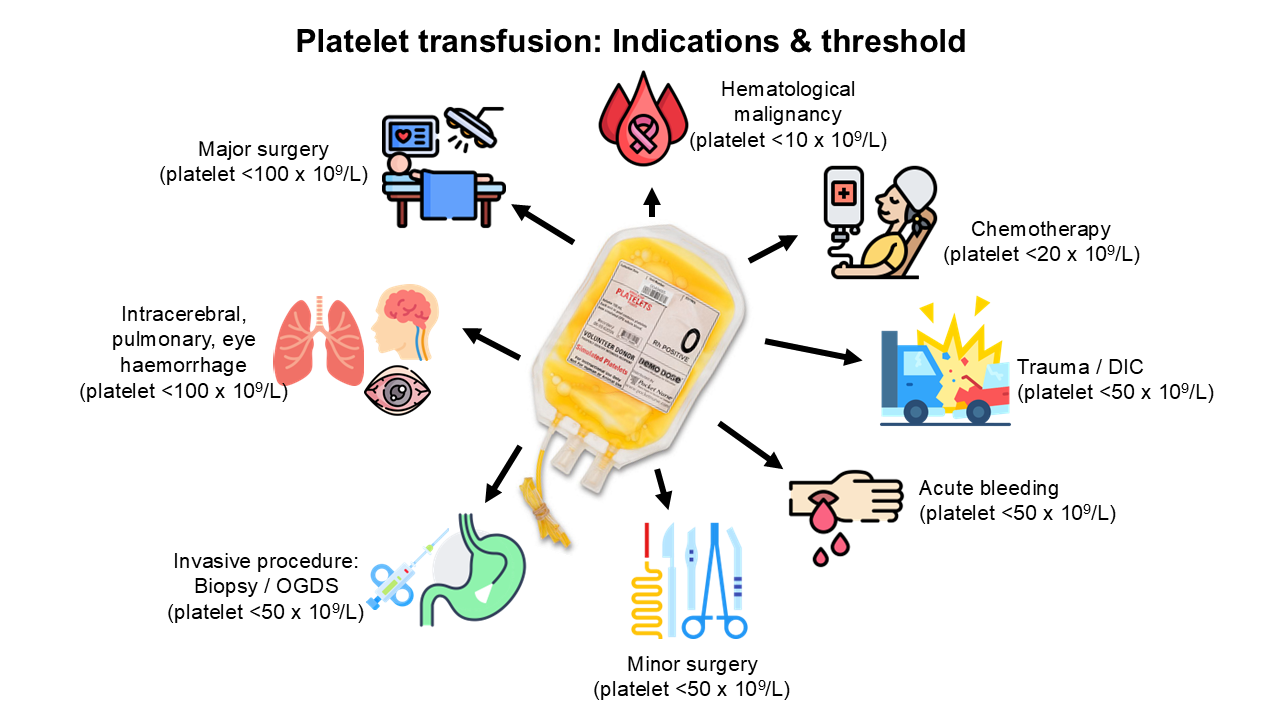
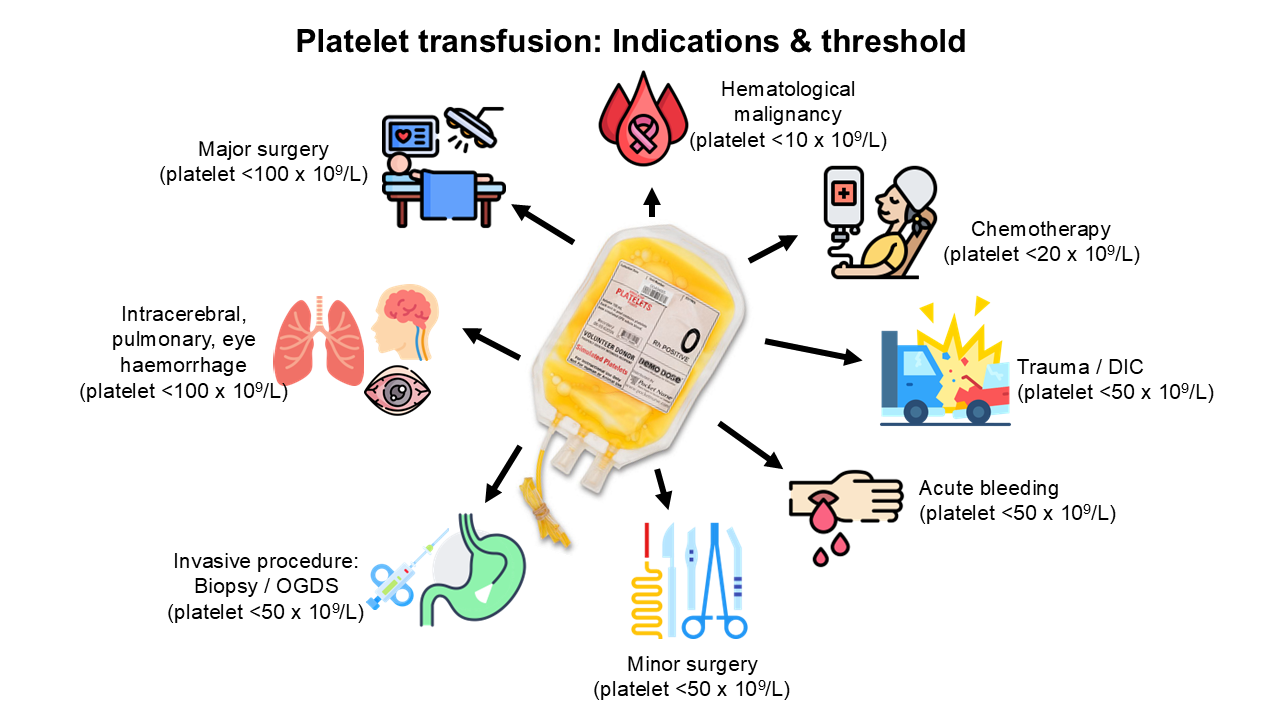
Indications for Platelet Transfusion
Platelet transfusion is primarily indicated to treat or prevent bleeding in cases of thrombocytopenia (low platelet count) or platelet function disorders. In hematological malignancies, platelet transfusion is indicated when the platelet count is below 10 x 109/L, except in certain conditions, such as fever, bleeding, or coagulopathy. If the patient requires chemotherapy or bone marrow aspiration and trephine (BMAT), the platelet count should be above 20 x 109/L.
In cases of acute bleeding, trauma, disseminated intravascular coagulation (DIC), or patients undergoing minor surgery or invasive procedures (e.g., lumbar puncture, oesophagogastroduodenoscopy (OGDS), or biopsy), the platelet count should be maintained to at least 50 x 109/L.
For patients with intracerebral, pulmonary, or ophthalmic hemorrhages, or those undergoing critical-site surgeries (e.g., eye, brain, or epidural procedures), platelet transfusion is indicated when the platelet count falls below 100 x 109/L.
Certain conditions contraindicate platelet transfusion, such as thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), and heparin-induced thrombocytopenia (HIT), as transfused platelets can exacerbate the condition. In these disorders, thrombi consume the transfused platelets, increasing the risk of thrombosis at critical sites. Platelet transfusion is also controversial in autoimmune thrombocytopenic purpura (ITP) and post-transfusion purpura (PTP), as transfused platelets are rapidly cleared by circulating antibodies, providing no clinical benefit.
Platelet transfusion in patients with renal disease (e.g., creatinine >265 µmol/L) is also controversial because transfused platelets may acquire the same metabolic and uremic defects causing platelet dysfunction. In these cases, platelet transfusion may be beneficial only during life-threatening bleeding.
Key Considerations for Platelet Transfusion
The decision to transfuse platelets must balance the potential benefits and risks. Repeated platelet transfusions can lead to platelet refractoriness, where the post-transfusion platelet count does not increase as expected. This occurs due to the development of antibodies against the human platelet antigen (HPA) or human leukocyte antigen (HLA), which destroy both patient and donor platelets. In such cases, HPA/HLA-compatible platelet transfusion or platelet crossmatching is recommended.
ABO-identical platelet transfusion is preferable to avoid the risk of alloimmunization due to the possible presence of PBC. However, it can be challenging for transfusion services to provide ABO-identical platelets to all patients due to the limited availability of platelet stock.
References
1. Handbook on Clinical Use of Blood. National Blood Centre, Ministry of Health, Malaysia. 3rd edition. 2020.
2. Agarwal A, Khan AI, Anwer F. Platelet transfusion. StatPearls Publishing. InStatPearls [Internet] 2024. https://www.ncbi.nlm.nih.gov/books/NBK560632/.
3. Dunbar NM. Does ABO and RhD matching matter for platelet transfusion?. Hematology 2014, the American Society of Hematology Education Program Book. 2020;2020(1):512-7.