This brings the question; how can we prevent being deferred from blood donation due to iron deficiency anaemia? Generally, this can be achieved with a few simple steps:
1. Iron-Rich Diet In the human body, iron is mostly stored in the red blood cells, forming the heme- portion of haemoglobin. Most of the iron is recycled from broken-down red blood cells, with the recommended intake for an adult being 8mg/day, while premenopausal women are recommended a daily intake of 18mg (5). The types of iron consumed can affect the absorption of iron.
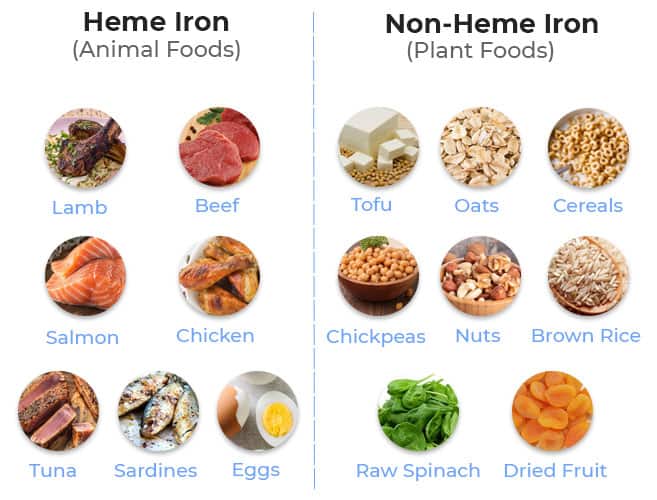
There are two forms of iron, namely heme and non-heme (Figure 2). Heme iron is available in meat, eggs, and seafood. This iron is more easily absorbed by the human body, up to around 30% of the food consumed. On the other hand, plant-based food such as vegetables, fruits, and nuts are rich in non-heme iron. Only around 10% of non-heme iron is readily absorbed by the human body, and this can be enhanced if consumed with vitamin C-rich food such as citrus fruits, peppers, and tomatoes (6).
Figure2 : Sources of Heme Iron and Non-Heme Iron
Source: https://vegansfirst.com/best-vegan-iron-supplements/
2. Avoidance of Dietary Antagonists of Iron Absorption One of the well-known inhibitors of iron absorption is calcium, therefore it is suggested to consume dairy products such as milk or calcium supplements at a different time than the main meals (7). Another antagonist of iron absorption is tannins, which are found in tea and coffee. Therefore, they should be avoided from being consumed with iron-rich food as well (7). Various timing suggestions have been made, such as avoiding food that limits iron absorption for at least 2 hours prior to or after a main meal that should consist of iron-rich food.
3. Iron SupplementationOral supplementation with iron can help certain at-risk groups such as vegetarians and young women, however, this must be accompanied by adequate knowledge of how to achieve the maximum effect of the iron supplements. They should be taken on an empty stomach (at least an hour prior to a meal), and best taken with a vitamin C-rich drink such as orange juice (8).
4. Donation IntervalsBlood donation itself would be a possible cause of iron deficiency anaemia among donors. Current guidelines would suggest an interval of at least 56 days after the previous whole blood donation. However, as per the National Blood Centre’s advice, it is suggested for an interval of around 3 months in between whole blood donations for the blood donors to recover the iron stores. This advice is in line with a study done in France, especially for donors with haemoglobin levels very close to the cut-off level (9).
In conclusion, iron deficiency anaemia is a major preventable cause of donor deferrals in Malaysia. Therefore, the general public, especially blood donors should be well informed on these simple steps to achieve the optimum iron stores.
References
1. Smith GA, Fisher SA, Dorée C, Roberts DJ. A systematic review of factors associated with the deferral of donors failing to meet low haemoglobin thresholds. Transfusion Medicine. 2013 Oct;23(5):309-20. Bahadur, S., Pujani, M., & Jain, M. (2011). Donor deferral due to anemia: A tertiary care center-based study. Asian journal of transfusion science, 5(1), 53–55. https://doi.org/10.4103/0973-6247.76001
2. Awaluddin SM, Shahein NA, Che Abdul Rahim N, Mohd Zaki NA, Nasaruddin NH, Saminathan TA, Alias N, Ganapathy SS, Ahmad NA. Anemia among men in Malaysia: A population-based survey in 2019. International journal of environmental research and public health. 2021 Oct 17;18(20):10922.Abd Rahman, R., Idris, I.B., Isa, Z.M., Rahman, R.A. and Mahdy, Z.A., 2022. The prevalence and risk factors of iron deficiency anemia among pregnant women in Malaysia: a systematic review. Frontiers in nutrition, 9, p.847693.
3. Trumbo P, Yates AA, Schlicker S, Poos M. Dietary reference intakes. Journal of the American Dietetic Association. 2001 Mar 1;101(3):294-. American Red Cross Blood Services, 2023. Iron Rich Foods. Available at: https://www.redcrossblood.org/donate-blood/blood-donation-process/before-during-after/iron-blood-donation/iron-rich-foods.html
4. Zander T. Iron Rich Vegan Foods [Internet]. 2022 [cited 2023 Aug 13]. Available from: https://vegansfirst.com/best-vegan-iron-supplements/
5. The Blood Safety and Conservation Team. Taking Iron Supplements: Information for Patients. Oxford University Hospitals, NHS Trust [Internet]. 2015 [cited 2023 Aug 13]. Available from: https://www.ouh.nhs.uk/patient-guide/leaflets/files/11903Piron.pdf
6. Baart AM, Van Den Hurk K, De Kort WL. Minimum donation intervals should be reconsidered to decrease low hemoglobin deferral in whole blood donors: an observational study. Transfusion. 2015 Nov;55(11):2641-4.