Restrictive Lung Diseases
Chronic respiratory diseases (CRDs) are diseases of the airways and other structures of the lungs as defined by the World Health Organization (WHO). In addition to tobacco smoking as the commonest aetiology, other risk factors for CRDs include aerosol-based environmental origin irritants like air pollution, occupational chemicals and dust, and frequent childhood respiratory infections. CRDs can subsequently be grouped into 4 major categories (Prezant et al., 2008):
I. Upper respiratory tract disease: Chronic rhinosinusitis and reactive upper airways dysfunction syndrome
II. Lower respiratory tract diseases: Reactive lower airways dysfunction syndrome, irritant-induced asthma, and chronic obstructive airways diseases (COAD/COPD)
III. Parenchymal or interstitial lung diseases: Sarcoidosis, pulmonary fibrosis, and bronchiolitis obliterans
IV. Cancers of the lung and pleura
The commonly occurred interchangeably among all 4 are lower respiratory tract and parenchymal lung diseases, or better known as obstructive and restrictive lung disorders with regards to their pathogenesis nature despite their almost similarities in pathophysiology. Hence, diagnosing them requires a lung function test to differentiate one another. Obstructive lung disorders are mainly bronchial asthma (BA) and chronic obstructive pulmonary disease (COPD), which later can be subdivided into chronic bronchitis “Blue Bloaters” and emphysema “Pink Puffers”. Whereas, restrictive lung disorders are interstitial lung disease, pneumoconiosis and sarcoidosis. Lung cancer and tuberculosis can be considered as restrictive in nature albeit the mixed picture presentation in diagnostic laboratory findings.
Restrictive Lung Diseases
People with
restrictive lung disease cannot fully fill their lungs with air. Their lungs
are restricted from fully expanding. In contrast to obstructive lung disease
which is characterized by swollen airway (thickening of the respiratory wall)
leading to bronchoconstriction (narrowing of respiratory passage) with
excessive production of mucus (stimulating chronic irritative bouts of
coughing) due to ongoing prolonged inflammation process, restrictive lung
disease is due to stiffening of chest wall tissue, weakened muscles or even
damaged respiratory nerves resulting difficulty in fully expanding the lungs,
thus more difficult to fill the lungs with enough air for respiration purpose
as demanded by the body. In short, obstructive lung disease is
a “clogged/narrowed” condition, whilst the restrictive type is
a “tight/stiffened” condition. Here are the examples of this type of
respiratory illness (Isa, 2020);
a) Interstitial lung disease: Idiopathic Lung Fibrosis (scarring of alveolar tissue).
b) Pneumoconiosis: Occupational dust; asbestos (Asbestosis) and silica (Silicosis).
c) Sarcoidosis: Autoimmune granulomas altering multiple organs’ structure and function.
d) Obesity: Obesity Hypoventilation Syndrome
e) Scoliosis: Abnormal “S”-shaped curvature of spine, resulting depressed chest wall shape.
f) Neuromuscular diseases:
g) Childhood muscular dystrophy (Duchenne and Becker)
h) Adulthood progressive motor neurons breakdown (Amyotrophic Lateral Sclerosis/ALS)
Lung function tests like spirometry
and peak flow meter are the ones able to diagnose a patient with the symptom of
exertional shortness of breath to be whether obstructive or restrictive in
nature. It is based on the parameters of Forced Vital Capacity/FVC (volume of
air forcibly blown out after a full inspiration) and Forced Expiratory
Volume/FEV1 (amount of air exhaled from the lungs in the first 1 second after
full inspiration). A low FEV suggestive of obstructive lung disease, on the
other hand, an addition of low FVC signifies restrictive lung disease.
Lung Cancer
Squamous Cell
Carcinoma (SCC) is the commonest type of lung malignancy, however,
Adenocarcinoma is trending in recent years. SCC is associated with male and
smoking prevalence, while Adenocarcinoma type is linked to female and
non-smoking populations. It is postulated that this fact is due to secondary
smoking (passive smoker) ‘culture’ existing at large within our very own
society. All together, any types of cancer are almost always in a linear
relationship with aging as evidenced through a Malaysian study (Liam et al.,
2006) stating the age of peak incidence of lung cancer is 7th decade
of life.
At clinical
stages I and II, patients are able to undergo curative surgical resection of the
tumor site of the lungs. Inductive therapy, in the form of chemotherapy or in
combination with radiotherapy, is applied to stages III and IV patients in
order to downstage the lung malignancy prior to curative surgical resection if
feasible based on the treating pulmonologist’s (respiratory physician) judgment
in agreement with cardiothoracic surgeon’s further evaluation.
Tuberculosis
Tuberculosis
is a chronic lung infection caused by Mycobacterium tuberculosis.
The mode of spread among humans is via aerosol droplet transmission hence the
lungs are often the focus of tuberculous disease although TB may present with the
disease in any organ system (Chakrabarti et al., 2007). In Malaysia, it is more
prevalent among the foreign labor workers and in deeply rural regions due to
incomplete as well as inaccessibility to BCG (Bacillus Calmette–Guérin)
vaccination program. Recent years of vaccine hesitancy movements worldwide
might just hamper the efforts done to eradicate this once contagiously fatal
illness. A cross-sectional study by Amaral et al. (2015) using data collected
from across the globe, concluded that tuberculosis is associated with a mixed
presentation of airflow obstruction and restrictive patterns on spirometry
assessment.
Exercise Testing for Pulmonary Disease
Submaximal
graded exercise test (GXT) is used to assess cardiopulmonary function and
fitness by providing an objective measure of exercise capacity, mechanisms of
exercise intolerance, prognosis, and disease progression and treatment
response. Modifications of traditional protocols depend on functional
limitations and the onset of dyspnea. Test duration of 8–12 min is optimal for
those with mild-to-moderate illness (Buchfuhrer et al., 1983), whereas a test
duration of 5–9 min is recommended for patients with severe and very severe
disease (Benzo et al., 2007). SpO2 monitoring must be done for these
patients as they may exhibit oxyhemoglobin desaturation with exercise, with the
maintenance of SpO2 > 90% is recommended.
However, individuals with pulmonary disease may have ventilatory limitations to exercise. Thus, prediction of VO2peak based on age-predicted HRmax may not be appropriate as criteria for terminating the submaximal GXT. The 6-minute walking test (6MWT) and shuttle walking test can assess functional exercise capacity in individuals with more severe pulmonary disease and in settings that lack exercise testing equipment. The use of bronchodilator therapy as a standby emergency medication is beneficial for such individuals. Exertional dyspnea is a common symptom in people with any pulmonary disease. The modified Borg Category-Ratio 0–10 (CR10) Scale (Figure 1) has been used extensively to measure dyspnea before, during, and after exercise (Ries, 2006). Patients should be given specific, standardized instructions on how to relate the wording on the scale to their level of breathlessness. In addition to standard termination criteria, exercise testing may be terminated because of severe arterial oxyhemoglobin desaturation. The exercise testing mode is walking or stationary cycling. Walking protocols may be more suitable for individuals with severe diseases who lack the muscle strength to overcome the increasing resistance of cycle leg ergometers. Arm ergometry may result in increased dyspnea that may limit the intensity and duration of the activity.
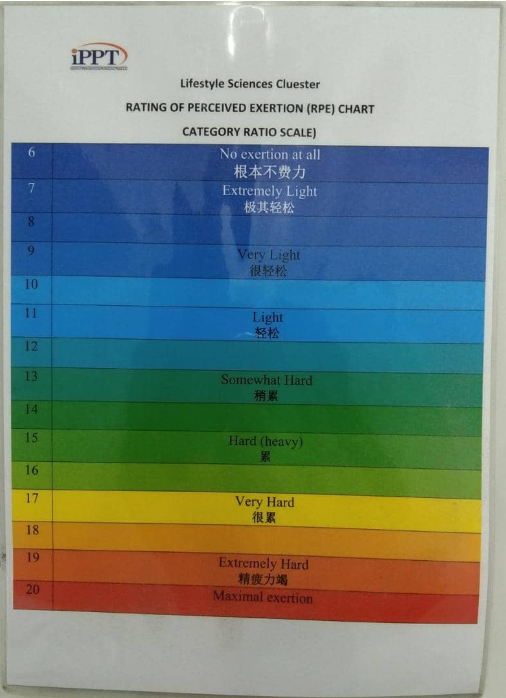
Figure 1: Modified Borg CR10 Scale for Dyspnea
Photo by IPPT
Exercise Prescription
Despite
substantially less investigation into the benefits of exercise training in
non-obstructive chronic lung diseases, strong scientific evidence supports the
inclusion of exercise training for many lung diseases other than Bronchial
Asthma and COPD with demonstrated clinical and physiologic benefits (Rochester
et al., 2014). However, the exercise programs should be modified to include
disease-specific strategies. Methods for adapting exercise training in patients
with restrictive chronic lung disease have been published (Holland et al.,
2013). Exercise training recommendations have been specifically presented for
patients with stable interstitial lung disease who are receiving optimal
medical management. For these patients, the FITT guidelines as below:
F: 3-5
day/week
I: Moderate
intensity. Intensities should be below those that would provoke severe dyspnea,
oxygen desaturation, or in some cases, hypertensive episode due to chronic
illness.
T: Morning
T: Aerobic
exercise should comprise the core component of the exercise program. Resistance
exercise training may be added after the aerobic training is established and
well tolerated.
Precautions:
Arm ergometry,
heavy resistance training, and pelvic floor exercise should be avoided to
reduce the risk of a Valsalva maneuver.
Apart from the
standard ACSM guideline meant for COPD, according to a local guideline by
National Cancer Society Malaysia (NCSM) issued in 2019; seated exercises are
the best form of training for lung cancer patient to build strength and
endurance, eliminating the risk of difficulty in breathing; with inhalation
during motion and exhalation when completing. This simple exercise steps can be
used for other restrictive lung diseases and tuberculosis patients as well, due
to its efficacy and safety with minimal effort without much exertion. The
seated exercise consists of:
1. Leg lift (alternating lift legs up to shoulders while sitting on a chair for 10 times)

Figure 2: Leg Lifts
Photo by Dr. Azizi
2. Seated kicks (kick foot off floor while sitting on a chair for 10 times)

Figure 3: Seated Kicks
Photo by Dr. Azizi
3. Overhead arm lifts (lift arms towards ceiling while sitting on a chair for 10 times)

Figure 4: Overhead Arm Lifts
Photo by Dr. Azizi
4. Windmills (circling arms while sitting on a chair for 10 times)

Figure 5: Windmills
Photo by Dr. Azizi
5. Pursed lip breathing is a good method to ‘retrain’ breathing regulation for lung cancer patients, simply by breath in through nostrils and slowly breath out through mouth by pursing the lips (like “blowing the candle” or “pulling out a thread from mouth”).
6. Buteyko breathing technique; a
nasal breathing (inhaling and exhaling via the nostrils) method; can be applied
as the exercise progresses, to control and prevent hyperventilation episodes
caused by the pulmonary diseases.
Special
Considerations
Peripheral
muscle dysfunction in the case of neuromuscular diseases (eg., Duchenne/Becker
and ALS) contributes to exercise intolerance and is significantly and
independently related to increased use of health care resources, poorer
prognosis, and mortality. Maximizing pulmonary function using bronchodilators
before exercise training in those with airflow limitation can reduce dyspnea
and improve exercise tolerance (Spruit et al., 2013). Inspiratory muscle
weakness is a contributor to exercise intolerance and dyspnea in those with
chronic lung disease. In patients receiving optimal medical therapy who still
present with inspiratory muscle weakness and breathlessness, Inspiratory muscle
training (IMT) , despite no clear guidelines for it, may prove useful in those
unable to participate in exercise training with an intensity of the training
load of at least 30% of maximal inspiratory pressure has been recommended
(Langer et al., 2009). IMT improves inspiratory muscle strength and endurance,
functional capacity, dyspnea, and quality of life which may lead to
improvements in exercise tolerance (Gosselink et al., 2011). Supplemental
oxygen is indicated for patients with SpO2 < 88% while breathing room air
(Qaseem et al., 2011). This recommendation applies when considering
supplemental oxygen during exercise. In patients using ambulatory supplemental
oxygen, flow rates will likely need to be increased during exercise to maintain
SpO2 > 88%. Although inconclusive, there is evidence to suggest the
administration of supplemental oxygen to those who do not experience
exercise-induced hypoxemia may lead to greater gains in exercise endurance
particularly during high intensity exercise (Nonoyama et al., 2007).
Individuals suffering from acute exacerbations of their pulmonary disease
should limit exercise until symptoms have subsided.
1) Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower
respiratory diseases after occupational and environmental disasters. Mt Sinai J
Med. 2008 Mar-Apr;75(2):89-100. doi: 10.1002/msj.20028. PMID: 18500710.
2) Liam CK, Pang YK,
Leow CH, Shyamala P, Menon AA. Changes in the distribution of lung cancer cell
types and patient demography in a developing multiracial Asian country. Lung
Cancer 2006; 53:23-30.
3) Chakrabarti B, Calverley PM, Davies PD. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2007;2(3):263-72. PMID: 18229564; PMCID: PMC2695198.
4) Amaral AF, Coton S, Kato B, Tan WC, Studnicka M, Janson C, Gislason T, Mannino D, Bateman ED, Buist S, Burney PG; BOLD Collaborative Research Group. Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J. 2015 Oct;46(4):1104-12. doi: 10.1183/13993003.02325-2014. Epub 2015 Jun 25. PMID: 26113680; PMCID: PMC4594762.
5) Buchfuhrer MJ,
Hansen JE, Robinson TE, Sue DY, Wasserman K, Whipp BJ. Optimizing the exercise
protocol for cardiopulmonary assessment. J Appl Physiol Respir Environ Exerc
Physiol. 1983;55(5):1558–64.
6) Benzo RP,
Paramesh S, Patel SA, Slivka WA, Sciurba FC. Optimal protocol selection for
cardiopulmonary exercise testing in severe COPD. Chest. 2007;132(5):1500–5.
7) Ries AL. Impact
of chronic obstructive pulmonary disease on quality of life: the role of
dyspnea. Am J Med. 2006;119(10 Suppl 1):12–20.
8) Rochester CL, Fairburn
C, Crouch RH. Pulmonary rehabilitation for respiratory disorders other than
chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(2):369–89.
9) Holland AE, Wadell K,
Spruit MA. How to adapt the pulmonary rehabilitation programme to patients with
chronic respiratory disease other than COPD. Eur Respir Rev.
2013;22(130):577–86.
10) National Cancer Society
Malaysia. 2019. Cancer & Physical Activity Booklet.
11) Spruit MA, Singh SJ, Garvey
C, et al. An official American Thoracic Society/European Respiratory Society
statement: key concepts and advances in pulmonary rehabilitation. Am J Respir
Care Med. 2013;188:e13–64.
12) Langer D, Hendriks E,
Burtin C, et al. A clinical practice guideline for physiotherapists treating
patients with chronic obstructive pulmonary disease based on a systematic
review of available evidence. Clin Rehabil. 2009;23(5):445–62.
13) Gosselink R, De Vos J, van
den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle
training in patients with COPD: what is the evidence? Eur Respir J.
2011;37(2):416–25.
14) Qaseem A, Wilt TJ,
Weinberger SE, et al. Diagnosis and management of stable chronic obstructive
pulmonary disease: a clinical practice guideline update from the American
College of Physicians, American College of Chest Physicians, American Thoracic
Society, and European Respiratory Society. Ann Intern Med. 2011;155:179–91.
15) Nonoyama M, Brooks D,
Lacasse Y, Guyatt GH, Goldstein RS. Oxygen therapy during exercise training in
chronic obstructive pulmonary disease. Cochrane Database Syst Rev.
2007;(2):CD005372.
Author(s):
Dr. Mohd Khairul Azizi Bin Mohd Zaki, MBBS (IIUM), IOC
Dip Sp Phy (Lausanne)
Dr.
Hazwani Binti Ahmad Yusof @ Hanafi, BSc. (UKM), MSc. (USM), PhD (Sydney)
MSc Clinical Exercise Science
(TCE508: Exercise Programming for Clinical Populations)
Lifestyle Science Cluster
AMDI, USM