Pre-deposit autologous donation (PAD) is a process in which patients donate their own blood before elective surgery, where significant blood loss is anticipated, such as in major orthopaedic, vascular, cardiac or thoracic surgery2.
PAD is typically indicated for patients with rare or multiple red blood cells antibodies that make crossmatching with allogenic blood difficult. It is also performed for patients whose religious beliefs prohibit allogenic transfusions. The donated blood is transfused only to the intended patient, reducing the risk of adverse transfusion reactions such as alloimmunisation and transfusion-transmitted infections. Furthermore, PAD provides fully compatible blood for patients with alloantibodies, offers reassurance to patients concerned about blood transfusion risks, and may also help conserve blood resources3.
Blood collection in PAD occurs three to five weeks before the planned surgical procedure. If more than one unit is required, donations can be made every seven days, and as frequently as every three days, up to 72 hours before surgery. The maximum number of units that can be collected is five. If the surgery is postponed, transfusion using the oldest autologous blood can be made and fresh blood can be collected3.
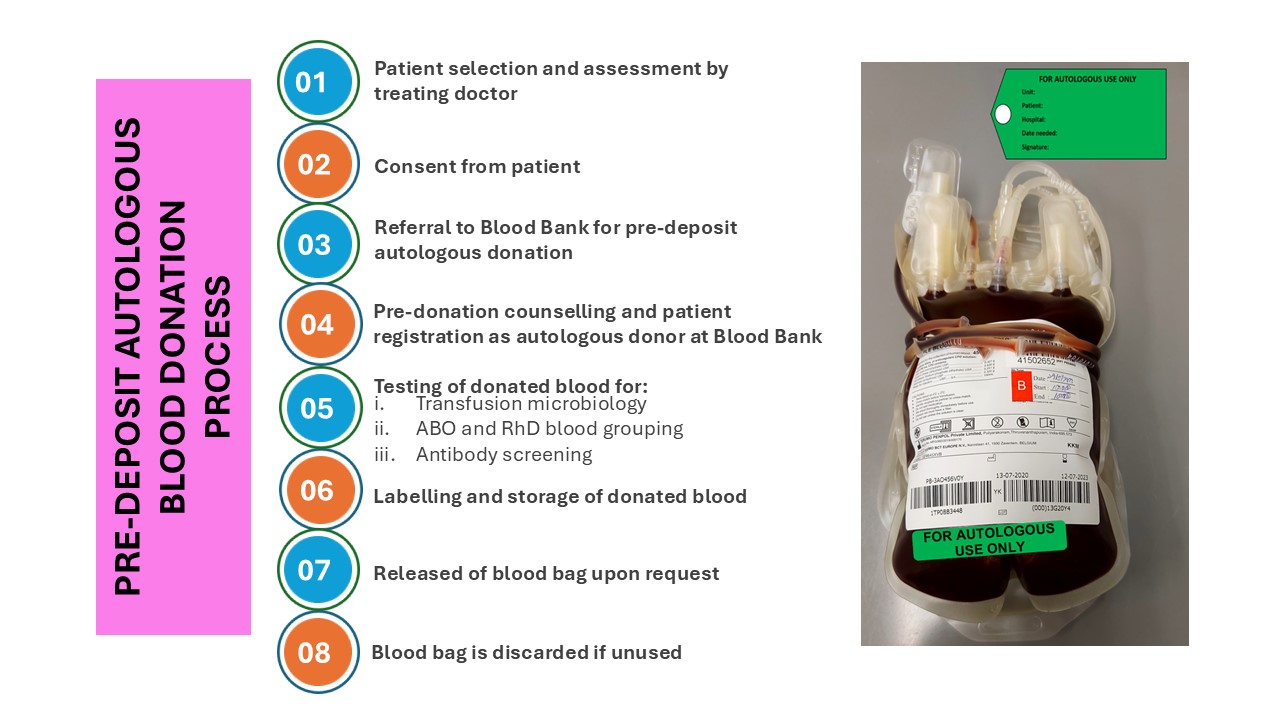
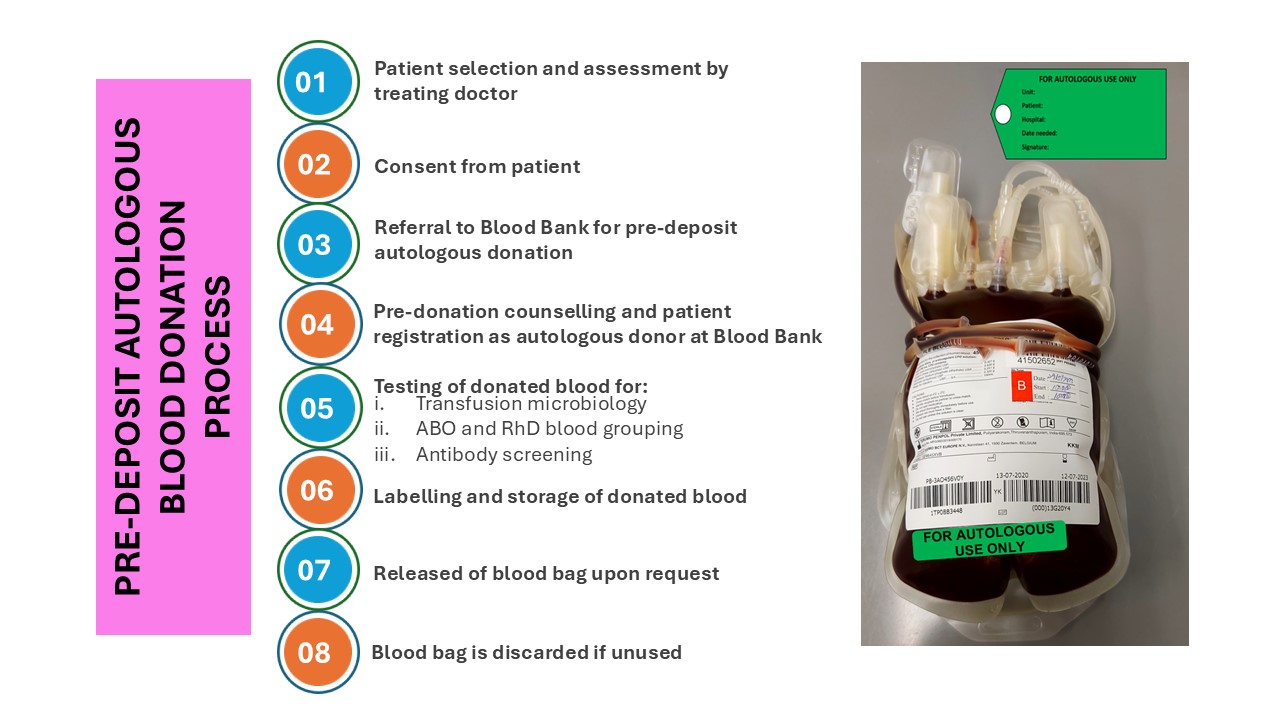
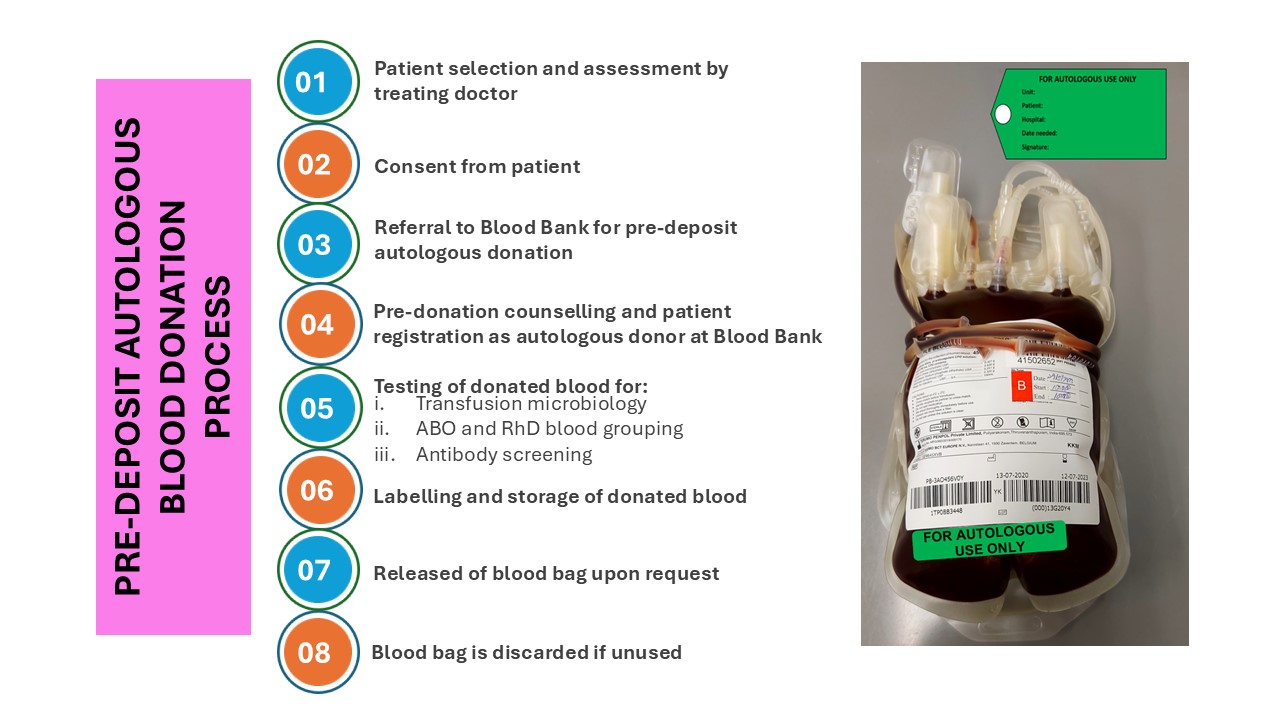
The treating doctor will determine the amount of blood to be collected and, consequently, the number of units required. The patient will be counselled by the treating doctor about PAD procedure and the risk that their donated blood may be discarded if unused. The patient must provide informed consent before donating blood. Subsequently, the doctor will issue a referral letter to the Blood Bank doctor for the donation process1,3.
The patient’s pre-donation haemoglobin level must be at least 11 g/dL for both men and women. Iron supplements, preferably administered via the intravenous route, should be prescribed before the first donation, and haemoglobin levels should be monitored before each subsequent donation to ensure they remain above 11 g/dL1,2,3.
Once the blood has been withdrawn from the patient, it will be tested for routine blood investigations, including ABO and RhD grouping, antibody screening, and transfusion microbiology screening (testing for HIV, hepatitis B, hepatitis C, and syphilis). If the blood tests positive for any microbiological agent, the PAD programme will be terminated. If the blood is non-reactive, it will be labelled with a green tag, and a tag stating "For autologous use only" will be attached to the blood bag. The blood bag will then be stored on a dedicated shelf or in a fridge within the Blood Bank to prevent it from being mixed with other blood bags in the inventory1,2.
The treating doctor must inform the Blood Bank and send the blood request form on the day of the operation so that the donated blood can be released to the patient. If the blood bag is not used, it will be discarded, leading to wastage1,2,3.
PAD collection is contraindicated in patients with certain underlying medical conditions, such as seizures, active systemic infections, a history of serious reactions to donations, and heart disease. Additionally, patients who test positive for infectious diseases, such as hepatitis B, hepatitis C, HIV, or other relevant infections, are not eligible for PAD1,4.
Currently, there is a reduced demand for PAD due to the availability of medications to treat anaemia and alternative techniques to conserve the patient’s own blood during surgery, such as blood salvage machine. However, PAD remains a valuable option in special cases where other approaches are insufficient4.
References:
1.Howard, Paula R.. (2017). Basic and Applied Concepts of Blood Banking and Transfusion Practices 5th Edition (5). Missouri: Elsevier Limited.
2.Harmening, Denise M.. (2019). Modern Blood Banking and Transfusion Practices (7). Philadelphia: F.A Davis.
3.Handbook on Clinical Use of Blood. National Blood Centre, Ministry of Health, Malaysia. 3rd edition. 2020.
4.Lynne Uhl, MD (2024). Surgical blood conservation: Preoperative autologous blood donation. UpToDate. https://www.uptodate.com/contents/surgical-blood-conservation-preoperative-autologous-blood-donation
SDG 3 - Ensure healthy lives and promote well-being for all at all ages