Apa itu Disleksia?
Disleksia dikategorikan sebagai masalah pembelajaran yang spesifik akibat neurologi dan genetik yang boleh diwarisi dari keturunan dalam keluarga. Ia dicirikan sebagai ketidak-upayaan memproses bunyi kepada bahasa tulisan yang mengakibatkan kesukaran untuk mengenali huruf perkataan dengan tepat, lemah kebolehan mengeja dan lemah untuk mentafsir atau men”dekod”kan perkataan tulisan dengan tepat dan lancar. Keadaan ini turut dikenali sebagai “Gangguan Pemprosesan Fonetik”. Kanak-kanak disleksia juga akan mengalami kesukaran untuk memahami tulisan bacaan yang boleh mengakibatkan gangguan pada perbendaharaan kata dan proses pembelajaran mereka. Disleksia tidak berkaitan dengan kecerdasan (IQ) ; individu dengan disleksia mungkin mempunyai IQ yang sederhana atau lebih.
Apa itu pemprosesan fonetik?
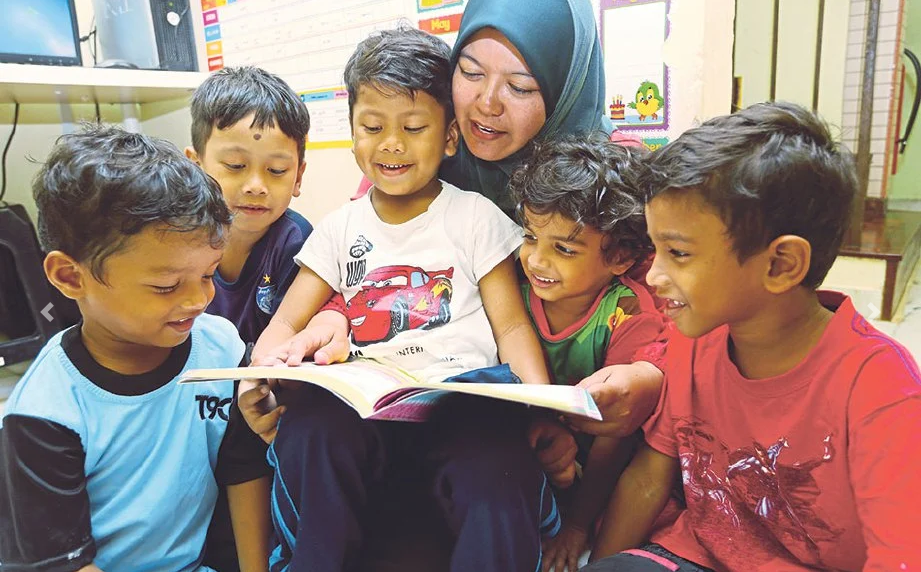
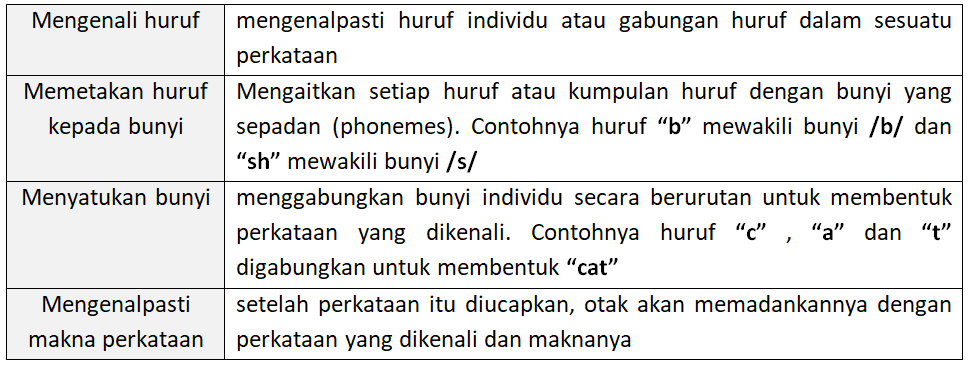
Pemprosesan fonetik adalah keupayaan menggunakan hubungan huruf-bunyi (letter-sound relationship) untuk membaca perkataan. Ia merupakan kemahiran asas dalam pembelajaran kemahiran membaca. Ia membolehkan individu menterjemah simbol tulisan (huruf dan kumpulan huruf) kepada bunyi yang sepadan untuk membentuk perkataan. Pemprosesan fonetik amat penting kepada kanak-kanak yang baru mula belajar membaca.
a) Membaca perkataan yang tidak dikenali dengan menggunakan peraturan yang sistematik
b) Membina kelancaran dan keyakinan dalam kemahiran membaca
c) Membangunkan asas kukuh untuk kemahiran membaca yang lebih maju seperti pemahaman.
Sebagai contoh, seorang kanak-kanak yang sedang belajar menemui perkataan “sand”. Dengan menyahkod atau mentafsir setiap bunyi /s/, /ae/, /n/ dan /d/ - mereka boleh menggabungkan bunyi-bunyi ini untuk menyebut perkataan dengan betul.
Apakah simptom-simptom Disleksia
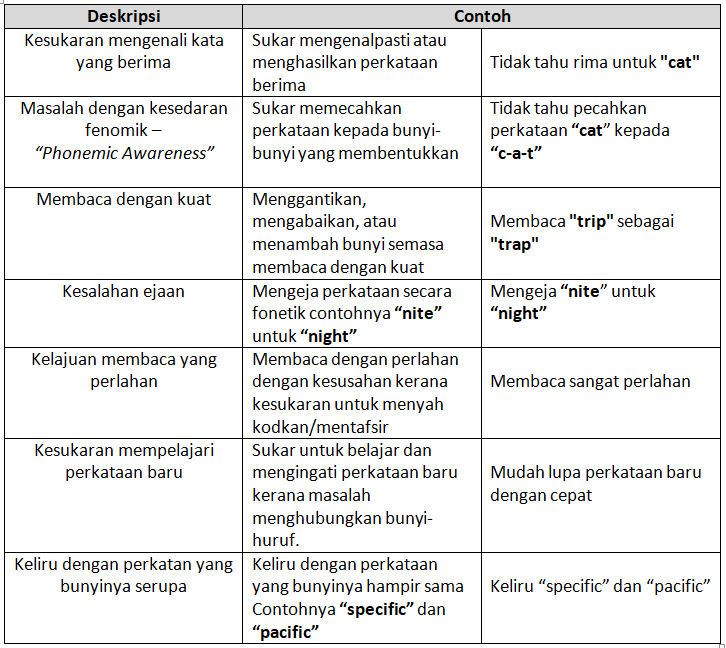
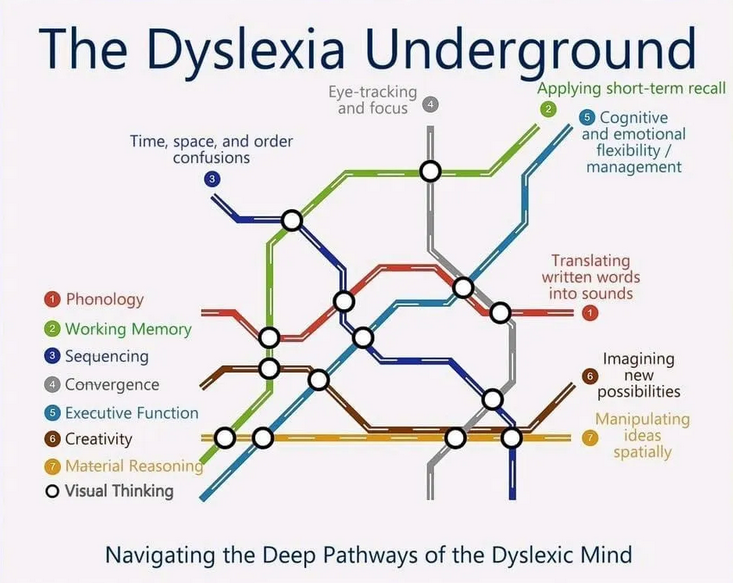
Walaupun banyak kajian dilakukan, kita masih belum mengetahui punca sebenar disleksia. “Gangguan Pemprosesan Fonetik” semata-mata tidak mencukupi untuk menjelaskan kepelbagaian ciri individu yang menghadapi disleksia. Terdapat pelbagai hipotesis gangguan disleksia (contohnya; “Phonological Deficit Model”; “Double Deficit Hypothesis”; “Visual Stress/Visual Deficit Model”; “Cerebellar Deficit Hypothesis”; “Magnocellular Deficit Hypothesis” ; “Auditory Deficit Model”; ”Multiple Deficit Model”; “Genetic Model of Dyslexia”; “Enviromental and Social-cultural models”). Kesemua hipotesis dan model-model penyebab yang dinyatakan masih diperdebatkan kerana tidak dapat menjelaskan semua gejala disleksia. Para pengkaji mengakui kompleksiti gangguan “neurodevelopmental” ini.
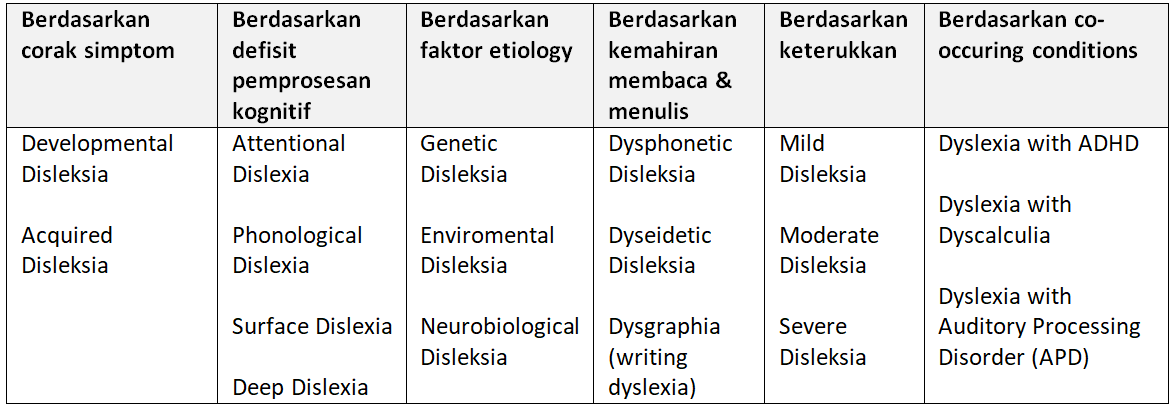
Subtype atau Jenis-jenis disleksia yang diketegorikan
“Phonological Dyslexia” mengalami kesukaran pada “Phonemic Awareness” dan pemprosesan fonetik. Mereka mengalami kesukaran untuk memecahkan perkataan kepada fenom, sukar mengeja dan menyahkod/mentafsir huruf. Fokus intervensi akan memberi penumpuan pengajaran berasaskan fenotik untuk menguatkan “phonemic awareness”.
“Surface Dyslexia”- Kesukaran mengenali perkataan sebagai unit keseluruhan “poor orthographic memory”. Mereka bergantung kepada menyahkod/pentafsiran fonetik menyebabkan kesilapan “irregular words” contohnya “yacht” akan disebut sebagai /yatch/. Membaca dengan perlahan dan sukar dengan “irregular words”.
Saya berharap pembaca tidak bimbang atau keliru dengan informasi yang diberikan. Maklumat di atas hanyalah untuk pengetahuan umum bagi pelajar atau pengkaji yang berminat dalam bidang pengkajian disleksia.
Bagaimana Diagnosis Disleksia dilakukan?
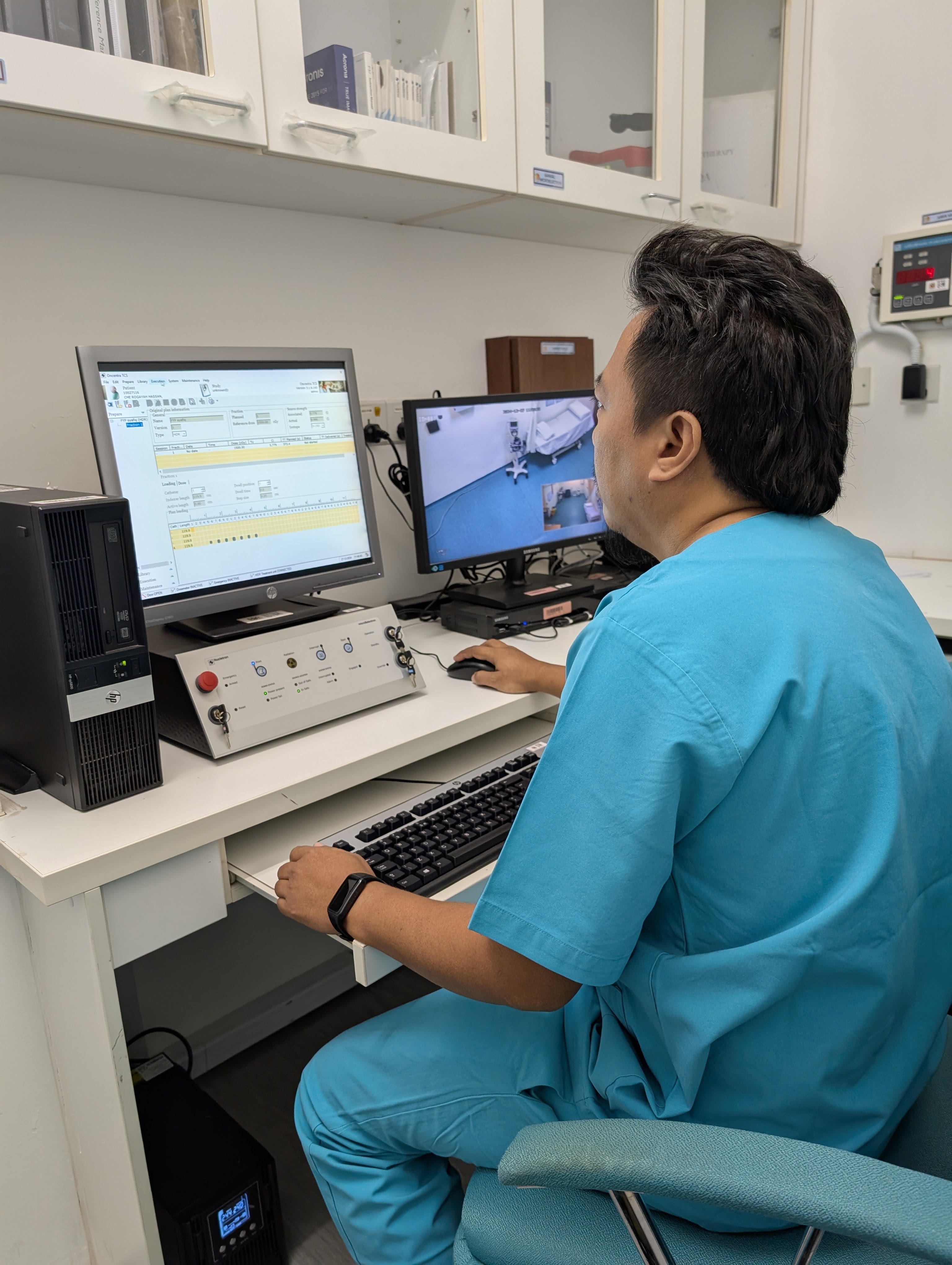
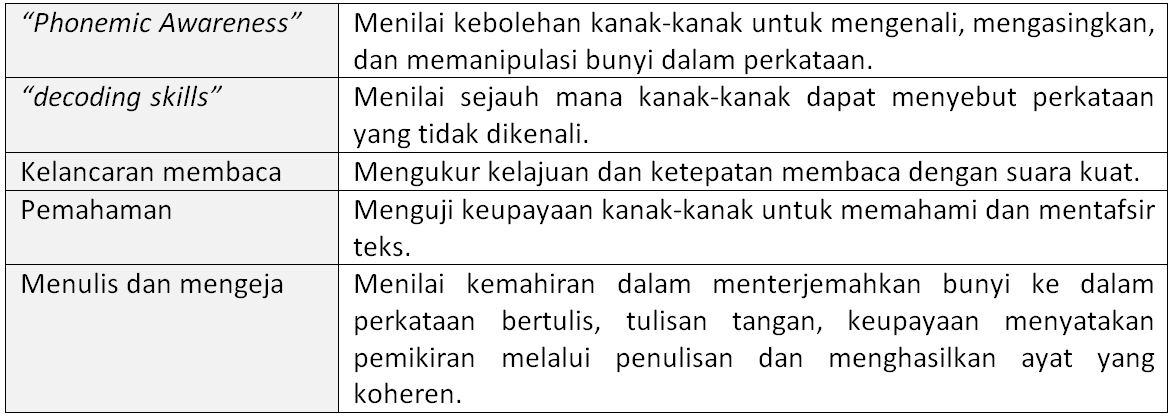
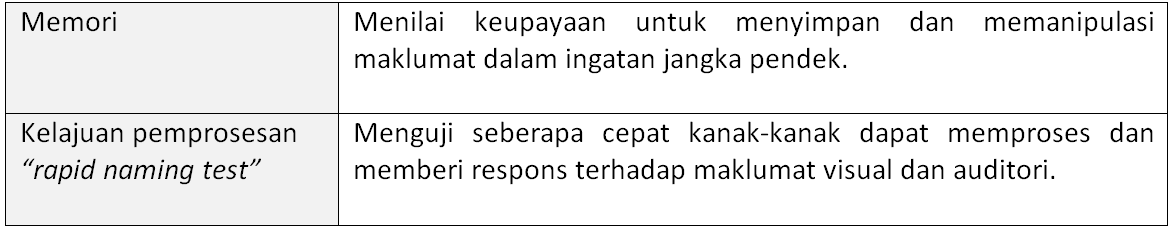
Untuk mendiagnosis disleksia ia akan melibatkan penilaian menyeluruh yang akan dilakukan oleh sekumpulan profesional yang terlatih termasuk pakar perkembangan kanak-kanak, klinikal psikologis, pakar pendidikan khas, ahli patologi pertuturan-bahasa. Proses ini akan melibatkan pemerhatian, temubual dan ujian perkembangan khas bagi menilai pelbagai aspek kemahiran membaca dan menulis, kemahiran lisan, pemprosesan fonetik, fungsi kognitif dan perkembangan kanak-kanak tersebut. Guru-guru atau ibubapa boleh segera merujuk kanak-kanak yang telah menunjukkan simptom-simptom disleksia. Walau bagaimanapun ada sekolah yang menjalankan saringan awal terhadap murid-murid yang berisiko menghidap disleksia.
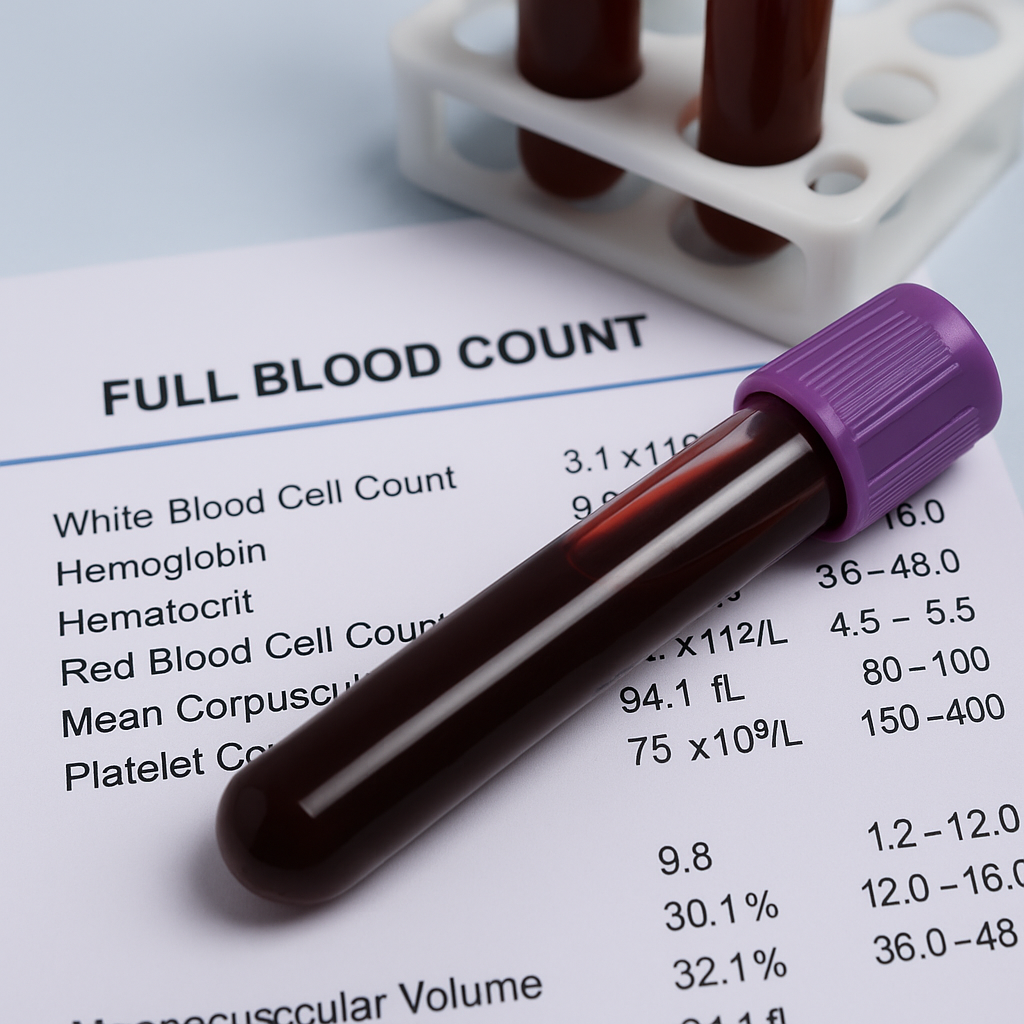
Temubual yang dijalankan akan melibatkan ibubapa dan guru-guru bagi mendapatkan sejarah perkembangan kanak-kanak, sejarah keluarga dan pengalaman pembelajaran kanak-kanak tersebut. Sejarah keluarga yang mengalami disleksia atau masalah pembelajaran lain kerana disleksia turut ada faktor warisan genetik. Amat penting untuk mengenal-pasti corak kesukaran akademik yang dihadapi dan juga tindak-balas intervensi yang mungkin telah dilakukan sebelum ini. Pemerhatian terhadap persekitaran kanak-kanak contohnya di bilik darjah, tingkah-laku, gaya pembelajaran dan interaksi mereka dengan rakan sebaya juga amat penting. Proses temubual dan pemerhatian ini bertujuan untuk melihat kemungkinan faktor lain yang menyumbang kepada kesukaran membaca seperti masalah penglihatan, pendengaran, kekurangan perhatian atau isu berkaitan emosi kanak-kanak. Berdasarkan pengalaman saya, kanak-kanak yang berhadapan dengan disleksia juga menghadapi cabaran emosi dan tingkah-laku seperti “anxiety” dan kurang keyakinan akibat kesukaran akademik. Faktor-faktor ini juga akan diambil kira dalam pelan intervensi nanti. Sesi penilaian atau ujian khas akan dilakukan untuk menguji komponen kemahiran membaca dan bahasa, komponen memori dan pemprosesan dan juga ujian kecerdasan (IQ).
Perlukan diingatkan proses yang disebutkan diatas mungkin sedikit berbeza berdasarkan pendekatan yang digunakan oleh profesional yang terlatih berdasarkan pengalaman masing-masing. Yang penting adalah pengesanan awal dan intervensi awal yang boleh kita lakukan kepada kanak-kanak yang menghadapi disleksia.
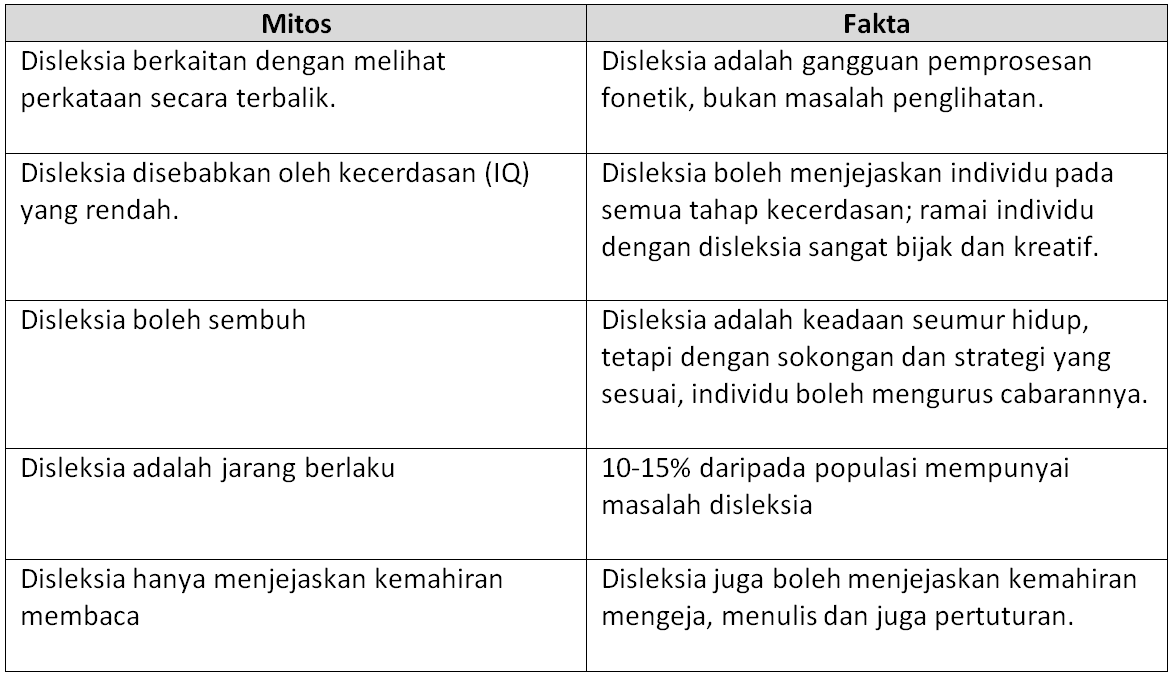
Mitos Tentang Disleksia
Bahasa Melayu mempunyai ortografi yang telus kerana terdapat padanan yang konsisten, satu-ke-satu antara huruf dan bunyi. Setiap huruf atau gabungan huruf biasanya mewakili satu bunyi, menjadikan perkataan lebih mudah untuk ditafsirkan. Sebagai contoh, perkataan “buku” dilafazkan tepat seperti yang dieja: /buku/. Kekonsistenan fonetik ini memudahkan proses penyahkodan/pentafsiran bagi pelajar disleksia dan mengurangkan beban kognitif yang diperlukan untuk membaca. Bahasa Inggeris pula mempunyai ortografi yang tidak telus, dengan peraturan ejaan yang tidak teratur dan hubungan yang kurang konsisten antara huruf dan bunyi. Sebagai contoh: Perkataan “read” boleh disebut sebagai /rid/ (present tense) atau /red/ (past tense). Perkataan seperti “though”, “through”, dan “thought” mengandungi corak huruf yang serupa tetapi mempunyai sebutan yang berbeza. Ketidak-konsistenan ini menjadikan bahasa Inggeris lebih mencabar bagi individu dengan disleksia, kerana ia memerlukan hafalan pelbagai peraturan dan pengecualian bahasa inggeris.
Dari segi kompleksiti fonetik pula, perkataan dalam Bahasa Melayu umumnya terdiri daripada suku kata yang mudah, sering kali dalam bentuk gabungan konsonan-vokal (KV). Kesederhanaan suku kata ini membantu pelajar disleksia dalam memecahkan dan menggabungkan bunyi. Bahasa Inggeris pula mempunyai struktur suku kata yang lebih kompleks, termasuk kelompok konsonan (contohnya perkataan; “strength”) dan huruf-huruf bisu (contohnya; “knife”). Kompleksiti ini, membebankan pelajar disleksia, menjadikan pemprosesan fonetik lebih sukar. Dari segi perbendaharaan kata dan perkataan, bahasa melayu mempunyai “irregular words” yang kurang. ”Irregular words” adalah perkataan yang tidak mengikuti peraturan fonetik atau ejaan standard sesuatu bahasa. Setelah pelajar disleksia menguasai pemprosesan fonetik, mereka boleh membaca kebanyakan perkataan Melayu dengan sedikit kesukaran. Bagi bahasa inggeris pula, mempunyai sejumlah besar “irregular words” (contohnya, “colonel”, “island”, “beauty”), yang memerlukan pelajar bergantung kepada hafalan berulang daripada pengekodan fonetik. Kebergantungan pada hafalan ini, boleh menjadi sangat mencabar bagi individu disleksia, yang sering menghadapi kesukaran dengan ingatan kerja.
Malaysia terdiri dari masyarakat berbilang kaum dan bahasa. Individu dengan disleksia akan terdedah dan mempelajari kedua-dua bahasa Melayu dan Inggeris. Sebenarnya, pendedahan dwibahasa ini boleh mempunyai kesan kepada mereka secara tidak langsung. Kesan yang positif: Ketelusan bahasa Melayu boleh membina keyakinan dan kemahiran literasi asas, yang mungkin secara tidak langsung menyokong pembelajaran bahasa Inggeris mereka. Namun kesan negatif pula: Beban kognitif mempelajari dua bahasa dengan sistem ortografi yang berbeza boleh menjadi sangat membebankan, terutamanya apabila beralih antara keteraturan fonetik bahasa Melayu dan ketidakaturan bahasa Inggeris.
Langkah-Langkah Yang Perlu Diambil Jika Mengesyaki Anak Menghidap Disleksia
Mengambil langkah proaktif apabila anak disyaki menghidap disleksia dapat memberikan perbezaan yang ketara dalam kehidupan mereka. Dengan intervensi awal, sumber yang betul dan persekitaran yang menyokong, kanak-kanak disleksia boleh mengatasi cabaran dan berkembang dengan baik dari segi akademik mahupun keperibadiannya.
1. Perhatikan tanda-tanda disleksia dengan teliti
2. Atur pertemuan untuk berjumpa dengan guru. Guru dapat memberikan laporan berkaitan prestasi anak terutama berkaitan kemahiran membaca dan menulis. Jika anak menghadapi kesukaran, dapatkan maklumat sama ada sekolah menawarkan program saringan atau intervensi asas
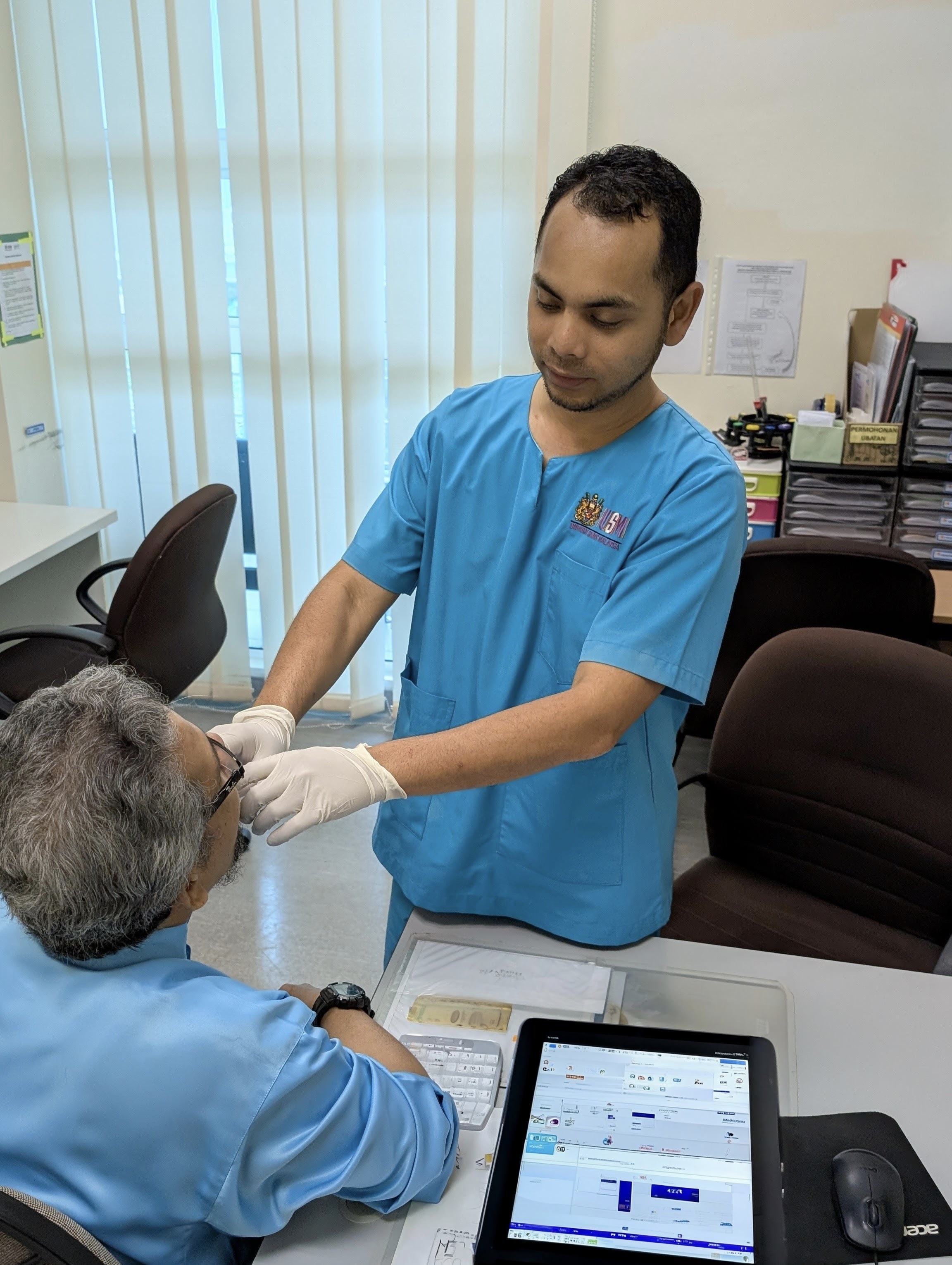
3. Dapatkan Penilaian Profesional Kesihatan sama ada di fasiliti Kementerian Kesihatan Malaysia ataupun di Pakar swasta. Kanak-kanak boleh dirujuk kepada hospital KKM melalui klinik kesihatan ataupun doktor umum (GP). Kanak-kanak tersebut akan di nilai oleh klinikal psikologis ataupun pakar perkembangan kanak-kanak. Selain itu terdapat Persatuan Disleksia Malaysia (https://dyslexiamalaysia.org/) yang turut menyediakan perkhidmatan saringan dan diagnosis disleksia
4. Fahami diagnosis Disleksia dan implikasinya. Selepas diagnosis disleksia telah dicadangkan kepada anak anda, pastikan anda memahami keputusan tersebut. Profesional kesihatan biasanya akan menggariskan cabaran dan kekuatan khusus kanak-kanak tersebut. Ibubapa boleh mendapatkan laporan yang merangkumi strategi pembelajaran dan pelan intervensi.
5. Ambil tahu “targeted” program intervensi yang ada di sekitar anda. Tidak semua sekolah awam menawarkan Program Pendidikan Khas Integrasi terutama disleksia. Ibu bapa diwajibkan mengemukakan surat diagnosis atau kad OKU kepada pihak sekolah tersebut. Pelan Pendidikan Individu (IEP) akan dibangunkan untuk anak tersebut. Terdapat juga terapi atau tuisyen persendirian swasta yang menyediakan program literasi berstruktur. Carilah tutor bertauliah yang terlatih dengan pendekatan pengajaran multi-sensori seperti kaedah Orthon-Gillingham. Alat bantuan pengajaran berteknologi seperti aplikasi “text-to-speech”, “audiobooks”, “reading pen” boleh membantu kanak-kanak disleksi mengatasi cabaran mereka sambil membina keyakinan diri. Terdapat peruntukkan undang-undang bagi menjamin hak kanak-kanak disleksia dibawah Akta Orang Kurang Upaya Malaysia 2008 dan dasar pendidikan Khas kementerian Pendidikan Malaysia. Bekerjasama dengan pihak sekolah bagi memastikan persekitaran pembelajaran anak disleksia adalah inklusif dan menyokong.
6. Berikan sokongan emosi kepada anak anda. Disleksia boleh menjejaskan keyakinan diri seorang kanak-kanak. Ibu bapa harus menyokong emosi mereka dan percaya ia bukan cerminan kecerdasan (IQ) atau potensi mereka. Raikan kejayaan kecil yang telah diraih oleh anak disleksi untuk meningkatkan keyakinan mereka. Galakkan mereka berkomunikasi secara terbuka tentang perasaan dan cabaran yang mereka hadapi.
7. Sertai kumpulan sokongan/ persatuan / jaringan. Saling berhubung dengan ibubapa lain yang mempunyai anak disleksia boleh memberikan sokongan emosi dan nasihat yang praktikal kepada ibubapa. Organisasi seperti Persatuan Disleksia Malaysia dan NGO sering menganjurkan bengkel, seminar untuk ibubapa. Banyak sumber ilmu yang boleh didapati sama ada secara bersemuka ataupun dalam talian. Ibu bapa juga harus menjaga komunikasi dengan guru-guru dan ahli terapi untuk memantau kemajuan anak masing-masing. Ibu bapa juga boleh menyumbang kepada usaha advokasi yang lebih luas untuk mendapatkan sokongan pihak kerajaan kepada kanak-kanak disleksia melalui kempen-kempen, menjadi sukarelawan dengan NGO yang boleh membantu kearah perubahan yang sistematik.