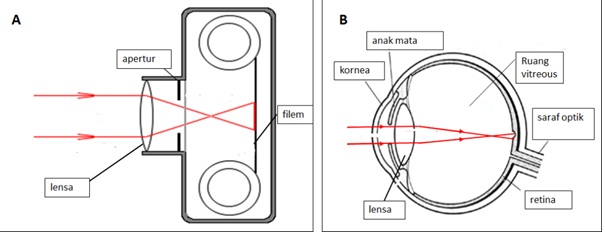
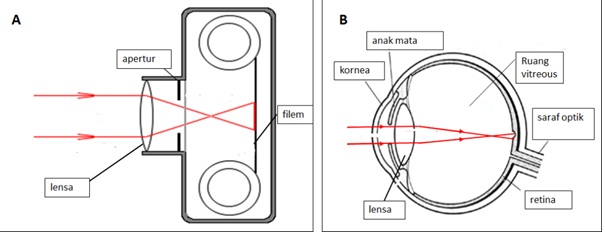
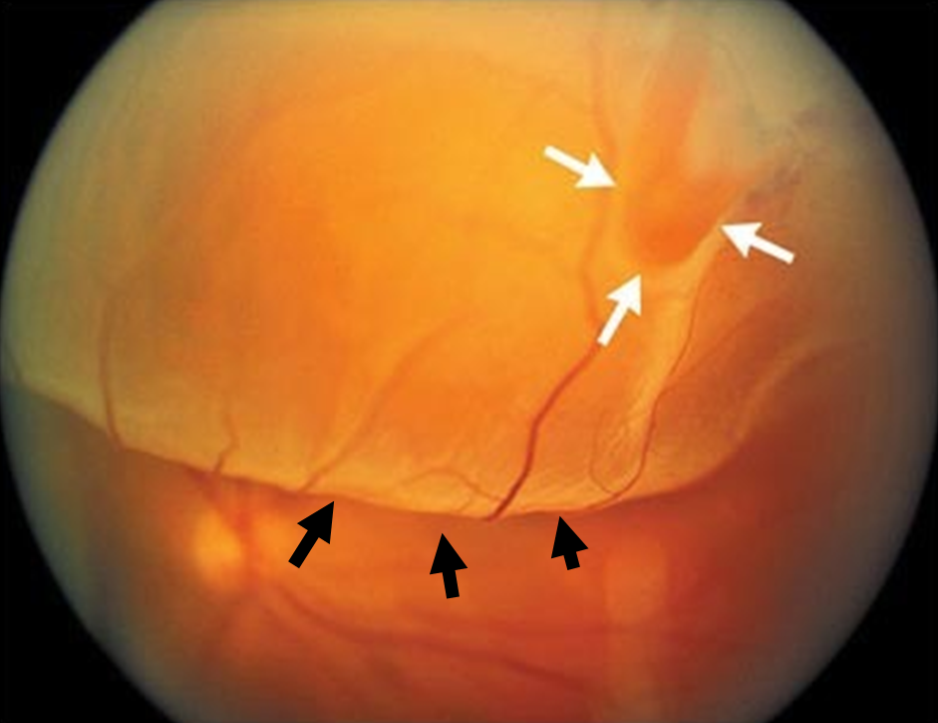
Ulangkaji struktur mata:


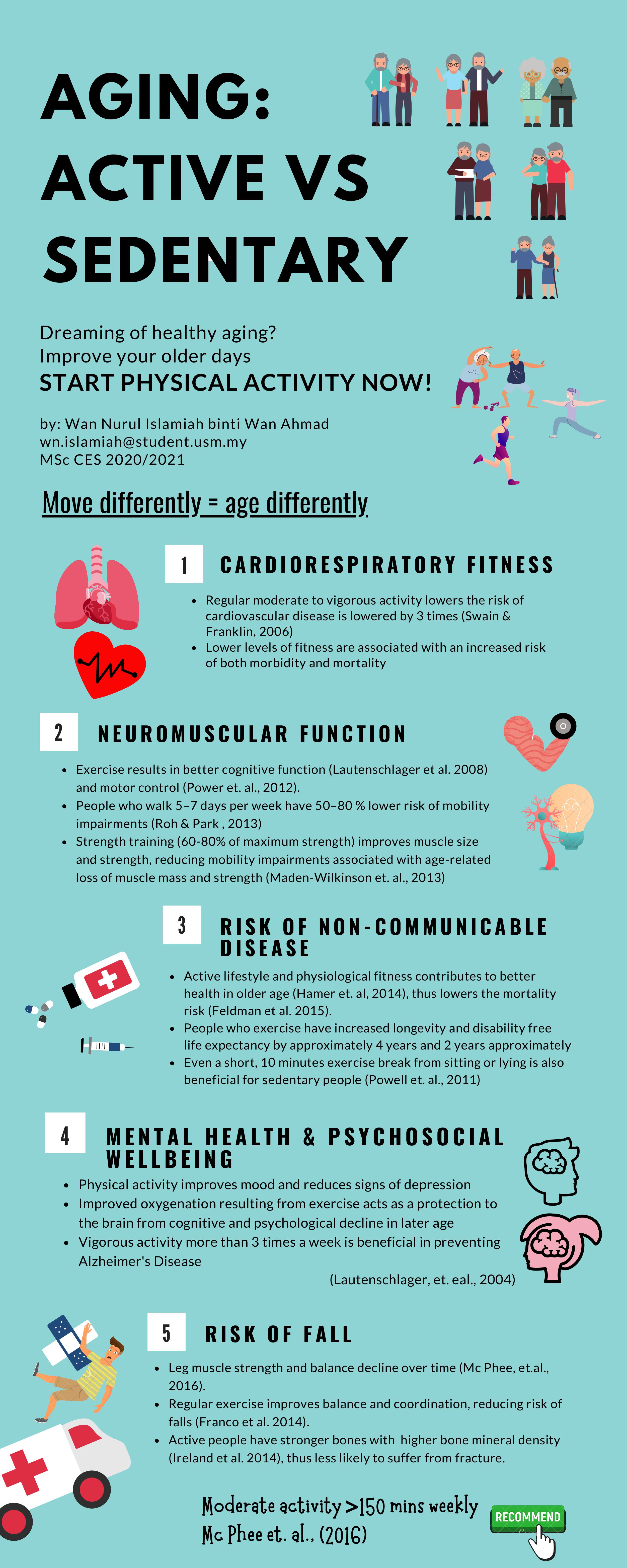
Aging
is the accumulation of physical changes over time. People said that if a person
spends much of the time napping then in the address book will the majority of
names that start with Dr, then there is likely that this individual might in
the aging period. As of the beginning of 2020, the percentage of the Malaysian
population aged 65 years and above has increased from 6.7% in 2019 to 7.0%.
Director of the National Institute on Aging (NIA), Dr. Richard J. Hodes said
that “People are living longer, but that does not necessarily mean that they
are living healthier”. Aging is not a disease, but it occurs at different
rates do not generally cause symptoms but the cellular and physiologic will
deteriorate over time which increased mortality with age following maturation,
increased vulnerability to disease, and decreased ability to adapt to stress.
Aging is affected by both intrinsic and extrinsic influences. Intrinsic aging
is the natural aging process. As we age,
the development of collagen decreases and cell turnover slows down. External
aging is caused by sunlight and stress that speed up the entire aging process.
Why Does Aging Happen?
Theories on aging have been around
for more than two thousand years. Ancient medical scientist, Galen believed
that aging is caused by the accumulation of waste matter in the body from the
beginning of life. These changes caused a slow increase in dryness and coldness
of the body. Meanwhile, Roger Bacon suggests a “wear and tear” theory that
aging is the result of abuses and insults to the body system. He suggests that
good hygiene might slow the aging process. In addition, Charles Darwin
attributed aging to the loss of irritability in the nervous and muscular
tissue. One of the popular aging theories is the Programmed senescence theory
that a process by which organisms through proceed physical deterioration of the
body. This theory proposed a degenerative process by which a cell loses its
ability to divide, grow and function which ultimately ends in death.
Age-related Physiological Changes
As we age, our sweat glands have
reduced production and heart rate, and skin blood flow will decrease as well.
The changes in the skin such as loss of subcutaneous fat that increase
vulnerability to pressure sores, less insulation of body to cold, and thickened
fingernails and toenails with some remaining pigment cells enlarge know as “age
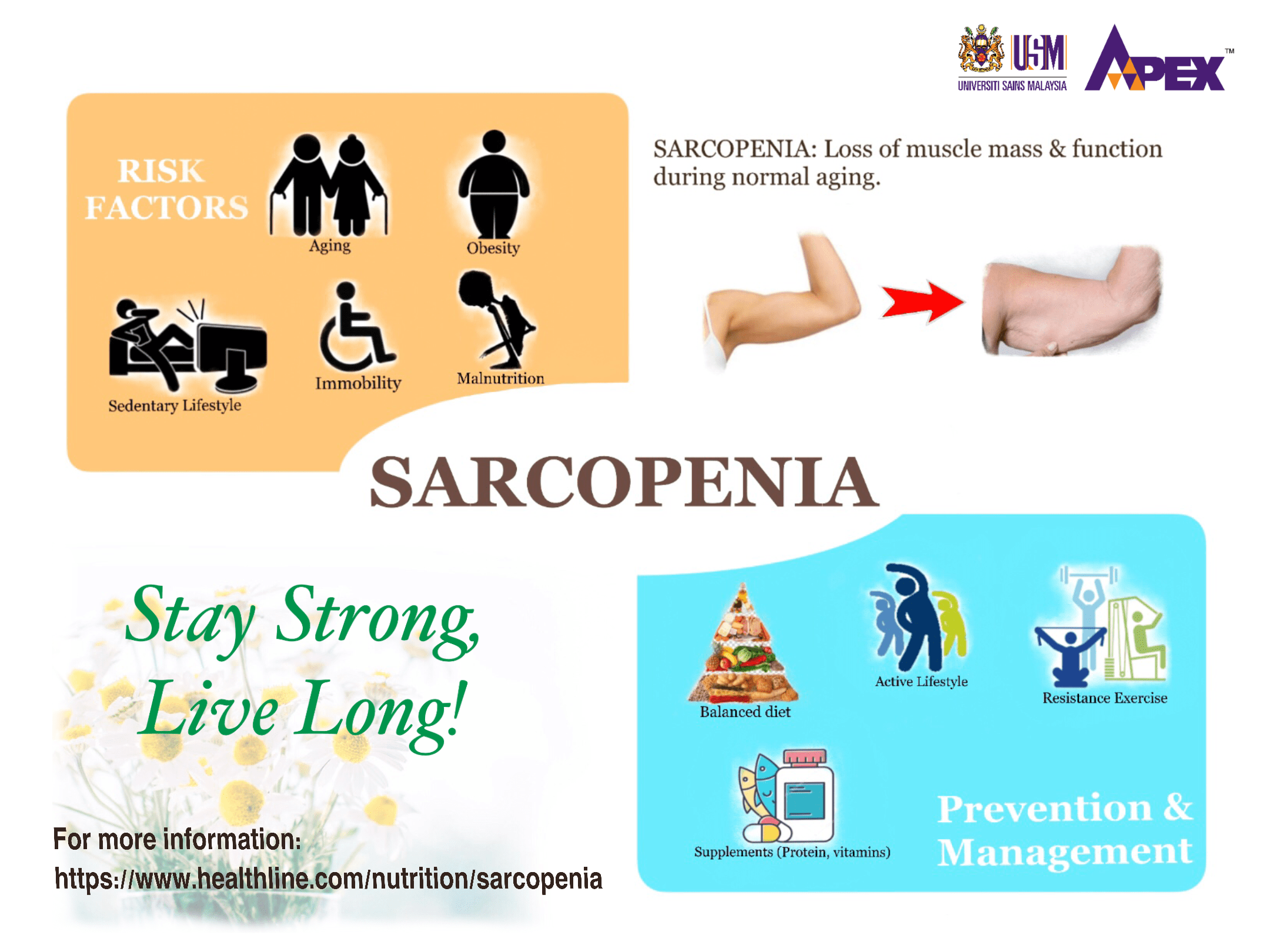
spots” will be obvious. There will also change in the musculoskeletal system
where the muscle mass will be decreased, deterioration in joint cartilage, and
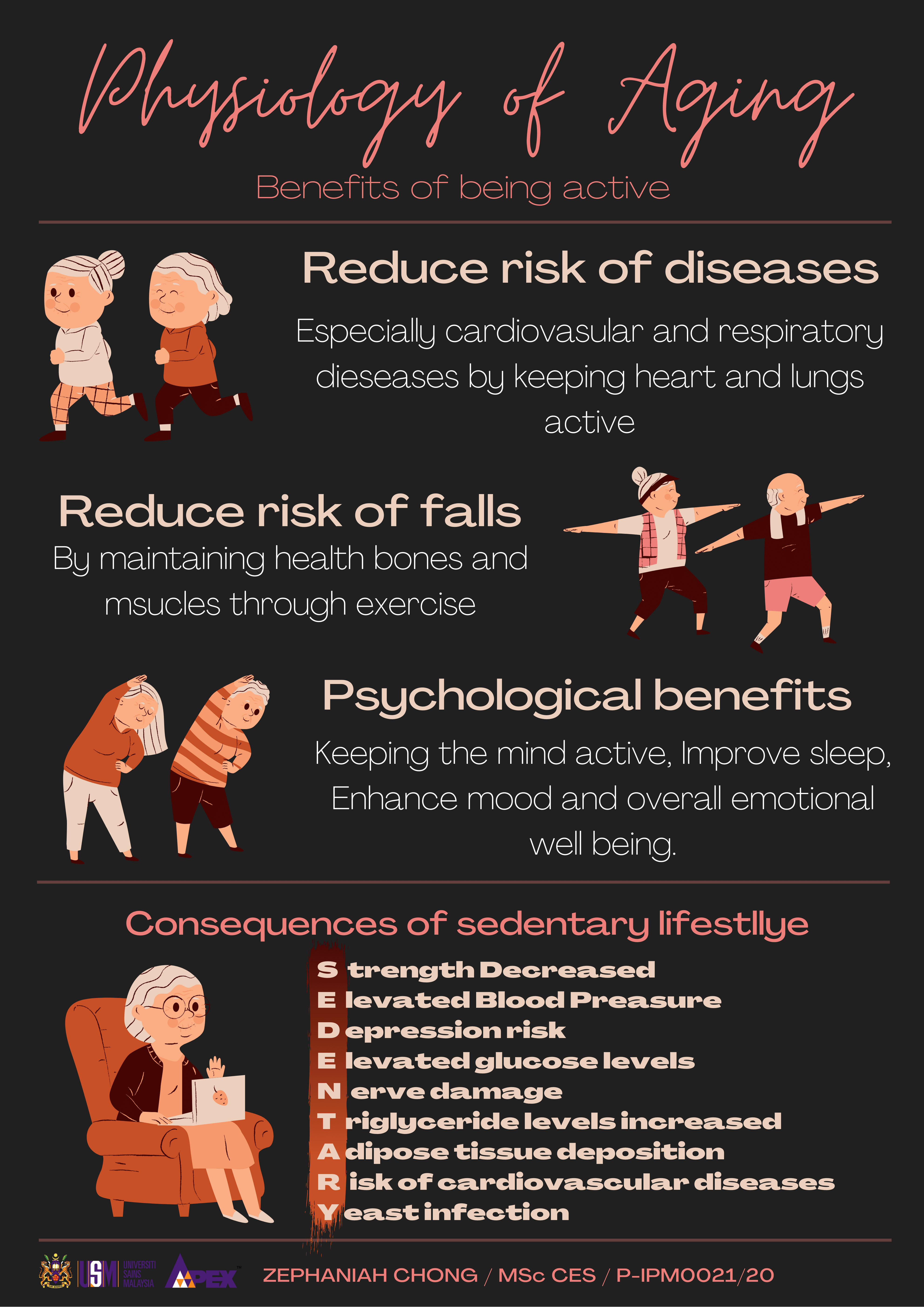
a decrease in bone density. All these changes, however, can be preventable or
reversible with regular physical activity.
Exercise
and aging
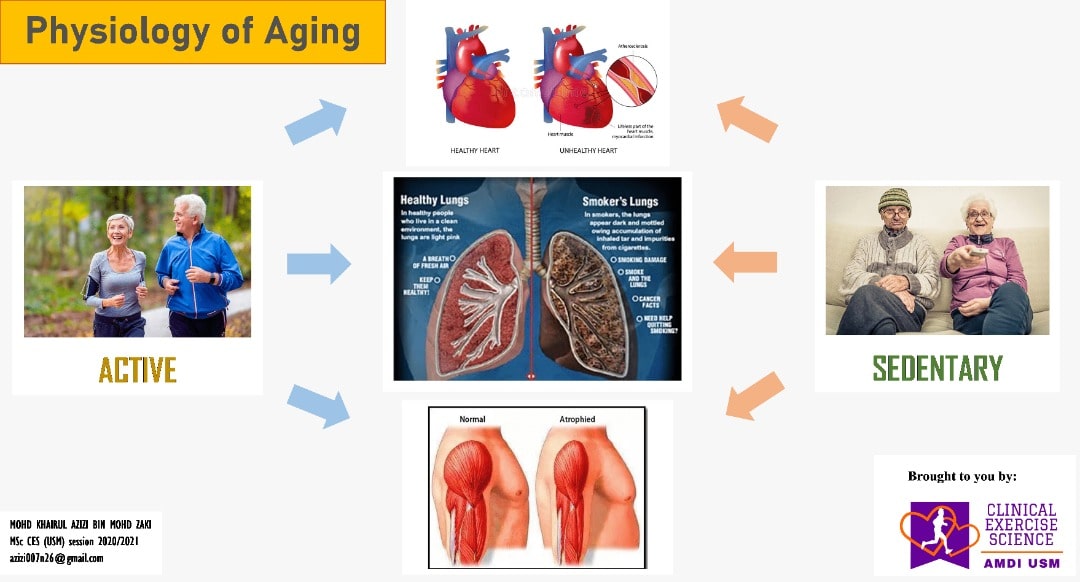
A person living a sedentary lifestyle is
often has a high risk for vascular aging due to reduction in vasodilation,
cardiac and arterial compliance, as well as endothelial dysfunction. However,
if a person living an active life, it will reduce the risk for vascular aging
due to less arterial stiffening and endothelial dysfunction. Many studies show
that a small change in physical activity or fitness in individuals who are
physically unfit or inactive can lead to a significant improvement in health
status, including a reduction in the risk of chronic disease and premature
mortality.
Exercise prevents cardiovascular disease
and death from the disease. The maximal oxygen consumption (VO2max) declines
with aging and is increased by regular exercise. VO2max is higher in trained
elderly persons and declines with age in both a trained and untrained elderly person
to become almost equal. Exercising at 45-50% of VO2max able to facilitate fat
loss and then start to metabolize carbohydrates that may decrease the risk of
diabetes. 12 weeks of high intensity and resistance training in younger and
older adults have shown that the oxidation capacity increased as well as
increased in muscle mass and strength.
Regular exercise helps to increase or
maintain control age or-related decreases in muscle mitochondrial mass and
antioxidant defenses. Exercise training can also result in 100% increments in
mitochondrial mass, oxidative (respiratory enzymes), and related enzymes for
defense against oxygen-free radicals. Studies have shown that gene expression
of Nrf2; a basic leucine zipper (bZIP)
protein that may regulate the expression of antioxidant proteins that protect
against oxidative damage triggered by injury and inflammation, and other
antioxidant defense genes were significantly increased in skeletal muscle of
fit males when partaking in exercise lasting more than 90 minutes. However, in
participants who had never exercised continuously, there were no effects on the
gene expression of Nrf2. The more we exercise, the greater this response comes,
and like everything, the body adapts to higher levels of stimulation to produce
antioxidants, so naturally, our body produces more even when at rest.
Sedentary people lose large amounts of muscle mass
(20-40%) and 6% per decade loss of Lean Body Mass (LBM). The aerobic activity
not sufficient to stop this loss. Only resistance training can overcome this
loss of mass and strength. Balance and flexibility training contributes to
exercise capacity. Aging appears neither to impair the ability to improve
muscle strength nor to prevent muscle hypertrophy. When older men (60 to 70 years
old) did strength training for 12 weeks at 80% of their one-repetition maximum
for extension and flexion of both knees, their extension strength is increased
by 107% whilst flexion strength increased by 227%.
What is the type of exercise that will
slow aging?
In the study “Resistance Exercise Reverses Aging in Human Skeletal Muscle’, it was proven that six months of progressive resistance training made the gene expression pattern of aging mitochondria become significantly younger. Scientists measured telomeres in twins to gauge the effect of exercise on aging, a study that proved the research participants who spent more than 3 hours each week lifting weights had longer telomeres than subjects 10 years younger, suggesting that individuals who eschew placing a vigorous load on their body may wind up biologically older by 10 years. Beyond the age of 30, we lose approximately six pounds of muscle mass per decade and these findings indicate that intervention designed to increase skeletal muscle mass (such as weight training) are critical weapons in the fight against obesity and obesity-related ailments, including diabetes, heart disease, stroke, hypertension, and cancer. Meanwhile, another study found that younger people participating in HIIT showed a 49-per-cent increase in mitochondrial capacity and the older group saw 69-per-cent. Mitochondria are the cells’ powerhouses, responsible for producing the molecule that transports chemical energy within cells.
Any kind of exercise is better than
none. Choose the one that you comfortable with. You know what is best for you.
Healthy life, long life!
The infographics simplified the exercise and aging as shown below.
Estebsari F, Dastoorpoor M, Khalifehkandi ZR, Nouri A, Mostafaei D, Hosseini M, Esmaeili R, Aghababaeian H. (2020). The Concept of Successful Aging: A Review Article. Curr Aging Sci. 13(1):4-10. doi: 10.2174/1874609812666191023130117.
By:
Hazwani Ahmad Yusof @ Hanafi,
Michelle Thang Ru Wen
Mohd Khairul Azizi Bin Mohd Zaki
Vishanth Rathakrishnan
Wan Nurul Islamiah Binti Wan Ahmad
Zephaniah Chong En Wei
Lifestyle Science Cluster, AMDI USM
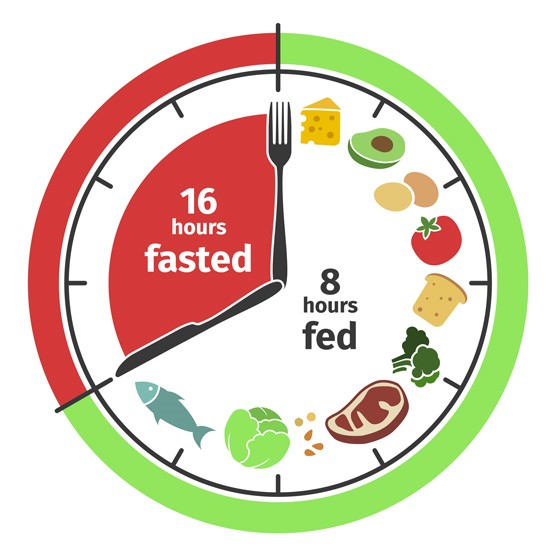
Gambarajah
1: contoh IF yang popular (16/8 Method)
As any religions existed in this world, there are certain conduct of practices performed as described in their own holy scriptures in refence to the commandments from God. The act of worshiping to The Creator symbolized the uniqueness of every religions embraced by different people; be it in the prayer recitations or the physical actions undertaken, apart from its theological belief. Islam, for one, has its very own prayer which is part of the 5 Arkanul Islam (Pillars of Islam) that served as mandatory foundation of a Muslim’s life; Shahada (Profession of Faith), Salah/Solat (Prayer), Zakat (Almsgiving), Sawm (Fasting during the month of Ramadan) and Hajj (Pilgrimage in Makkah al-Mukarramah, if able).
Solat is the daily obligatory prayers observed five times a day at prescribed times namely; Fajr (dawn), Zuhr (afternoon), Asr (evening), Maghrib (dusk) and Isya’ (night). It composes of repetitive cycles (Raka’ah) of 5 differing main postures listed below;
Takbir: raising both hands, thumbs parallel to earlobes with God magnification chant.
Qiyam: standing with right hand on top of left hand, affixed at chest to below navel.
Ruku’: bowing with hip flexion at 90o angle, head facing down.
Sujud: prostration in submissiveness with only face, hand palms and toes in contact with floor.
Julus: sitting/kneeling with buttocks rest on heels, plantar-flexed feet and hands on laps.
Given the different movements performed in Solat, it may imitate the functional exercise.
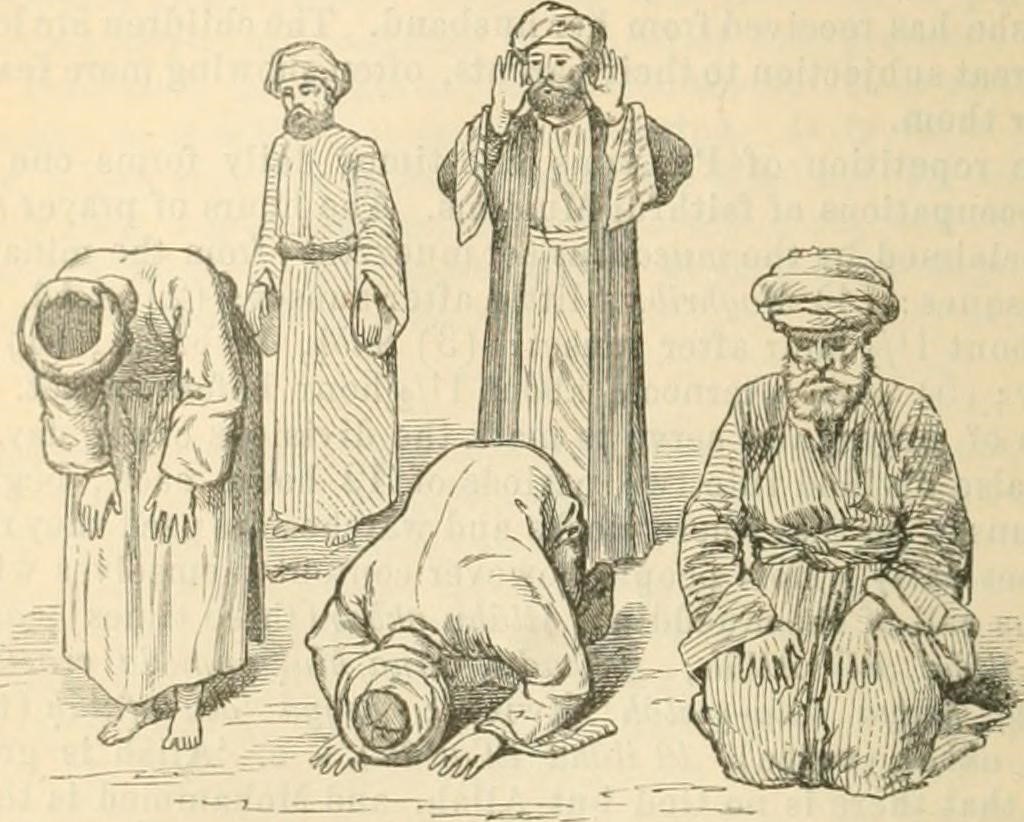
Figure 1: Postures in Solat
(Source: Google Image)
So, what is functional exercise? It can be defined as movements incorporated in exercise regime to improve an individual’s ability to perform daily activities and achieve specific goals. The main goal is to enhance living function in normal daily life especially among clinical and physically-disabled populations. The functional exercise training principles can be based on the 3-dimensional (3D) planes of motion; transverse, sagittal and frontal, involving series of muscular contractions (isometric and isotonic) and focuses on the 4 pillars of human movement;
I. Locomotion: linear displacement of body mass.
II. Level changes: non-locomotor up and down motion.
III. Pushing/pulling: daily eccentric/concentric motions.
IV. Rotation: truncal pivoting movement in changing direction.
Faith-Fitness Relationship
Taking the basic principles of functional exercise in mind, it is observed that performance of Solat utilizes numerous level changes and pushing/pulling motions with slight rotation at the end of the prayer via Taslim (a minor but important prayer movement of giving Salam by turning head to the right and then left). It can be said that Solat is inadvertently a form of functional exercise on its own, performed for five times on daily basis by Muslims worldwide. Solat involves continuous gentle muscle contraction and relaxation with recurring range of motions (ROMs) involved in perfect harmony and balance, by employing different types of stretching and isometric contractions, and is generally suitable for all ages & conditions.
Surprisingly, a collaborative study between Departments of Cardiology and Biomedical Engineering, Universiti Malaya (UM) in 2008 which produced an enlightening book titled “Salat: Benefits from Science Perspective” found that 12 Raka’ah (combination of Zuhr, Asr, and Isya’ prayers) is equal to 30 minutes of light exercises daily as recommended by the American College of Sports Medicine (ACSM) guideline used worldwide. Dr. Jaseem Ramadan Alkandari from Kuwait, in his remarkable 2007 study “Bioenergetics of Islamic Prayers”; concluded that Solat does have positive effect on metabolic function as well via the energy cost of about 80 calories a day from daily prayers for an 80 kg person, and it could be considered a form of physical activity that enhances fitness.
Specifically, Fatimah Ibrahim & Siti A. Ahmad (2012) investigated Takbir, Ruku’ and Sujud postures via electromyography (EMG) output, comparing them to similar stretching exercises and suggested that Solat has musculoskeletal effect-like stretching. Takbir stretches the Pectoralis (chest) muscles and shoulder blades gently as a start-up motion signaling into next posture progression. Even weight distribution via both feet is observed throughout the practice of Qiyam posture, easing the balance of the body and lower back in a neutral position whilst activating the core muscles at the same time. This correct standing position aids to straighten the back and improves posture (Winter DA, 1995). Ruku’ is a form of loading exercise which strengthens the back, extends the spine and increases the flexibility of hips and hamstrings, thus relieving the stiffness at spine, neck, and back, and helps to improves posture as well as balance and co-ordination. This position stretches the para spinal muscles of lumbar spine, hamstrings, and calves (gastrocnemius & soleus) muscles. It is useful to treat backache for chronic back pain patients or even pregnant mothers (Aqlan F et al., 2017) and vertebral column related diseases, as well as enhancing bone health by minimizing the risk of Osteoporosis (weak, brittle bones).
Spinal stretch is maximized through Sujud posture as a person curls the torso over the legs creating a space between the dorsal surfaces of the vertebra of the spine and aids spinal distraction as well as allowing neural glides and the lengthening of the nerves (Shacklock M, 2005) which is important to treat spinal stenosis and other degenerative disc diseases (Ji B et al., 2003). This movement also utilized the level changes as evidenced by the head is in the position lower than the heart, reducing the blood pressure and ultimately, chances of stroke in later time. Julus sitting in kneeling position strengthens the core muscles, hence maintaining good posture and improves the flexibility of knee joint ligaments as well as tibialis anterior (shin), extensor hallucis longus (toes), the quadriceps (thigh) and gluteus (buttocks) muscles. Rising up after Julus to proceed with another Raka’ah of prayer involves deep squat motion, which emphasized more on spinal stability. The head turning motion in Taslim stretches the trapezius muscles, mobilizes the upper back and thoracic muscles over the cervical vertebral column. These gentle neural stretches at cervical rotation are effective and may reduce the symptoms of cervicogenic headache, the likelihood to suffer from cervical spondylosis or myalgias (Al-Gazal et al., 2008).
Between ROM (Range of Motion) and RM (Ritual Movement)
A comparison being made between Yoga and Solat by Sayeed SA and Prakash A in a 2013 Indian study on the togetherness between these dominant practices of fitness and faith respectively in mental health. It is concluded that there are resemblances in Solat and Yoga postures which simultaneously can give similar benefits, thus, suggesting Solat as an alternative to the current existing flexibility-cum-core strengthening exercises like Yoga and Pilates. Ghazal Kamran; a senior physiotherapist in Rehabilitation and Physical Medicine Institute, Al Ain Hospital (UAE), elaborated concisely in 2018 about the similarities between Solat and Yoga along with their therapeutic effects. It is worth to note that the main 4 postures from Solat ritual (Qiyam, Ruku’, Sujud and Julus) closely resembled that of some Yoga postures respectively;
Namaste (“Bowing to you”): standing, hands together at chest, bowing head with eyes closed.
Ardha Uttansana (standing half forward bend): fully stretches the muscles involved in Ruku’.
Balasana (Child pose): helps in releasing the tension in the lower back, shoulders and chest.
Vajrasana (Thunderbolt pose): gets rid of constipation and improves blood flow circulation.
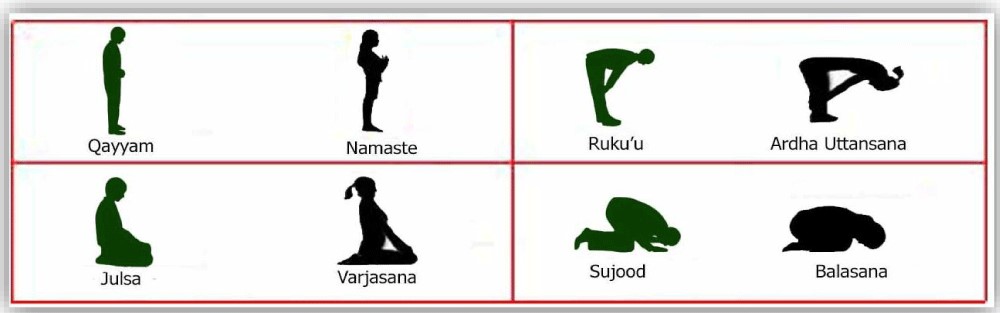
Figure 2: Similarities in Solat and Yoga Postures.
(Source: Kamran G. Physical benefits of (Salah) prayer - Strengthen the faith & fitness.)
Bear in mind that any flexibility training involved stretching activities, hence, one must be able to relax or be in a ‘state of calmness’ first before being able to perform the stretches as it might leads to injury. This ‘state of calmness’ formed the basis of clear mind, inwardly focus and leaving out all worldly life distractions for both Yoga practice and Solat ritual. Based on the mechanical properties of connective tissues (muscle) in our body as a protective mechanism from the Stress-Strain component, it can be divided into elasticity (ability to return to normal), plasticity (permanent change after force is applied) and viscoelasticity (resisting changes but unable to return to normal). Solat falls within the elasticity phase in the Stress-Strain Curve which enabled our body components stretched return back to normal state. Most Solat postures lasted within 10-30 seconds (as per ACSM safe guideline in stretching activities), coinciding with the recitations and momentarily pauses specific to different ritual movements.
Prostration, by its sociocultural nature alone, is an act of submission to a higher-ranked person, victor of a battle or in the case of Solat, to the highest-being God the Almighty; in favor of mercy from Him. Sujud is the only Solat position in which the head is positioned lower than the heart and therefore, receives increased blood supply to the brain, stimulating the brain’s prefrontal cortex which houses the higher thinking order (aql) enabling it to control emotions from the limbic system (nafs) spiritually. This surge in blood flow has a positive effect on memory, concentration, psyche and other cognitive abilities. The prefrontal cortex is located in the frontal lobe which contains the most dopamine neurons. Dopaminergic pathway is exclusive in synthesizing and releasing the dopamine hormone which is essential in activating parasympathetic nervous system to conserve energy and stays in ‘rest mode’. In other words, dopamine is a calming hormone which gives human the feel-good sensation physically and psychologically. It is stipulated through a study (Doufesh, 2012) investigating the increased amplitude of alpha brain activity during prostration in the parietal and occipital regions suggestive of parasympathetic elevation, thus indicating a state of relaxation.
Increment of dopamine increased the protective effect against anxiety disorders and Parkinson’s Disease; which are caused by lack of dopamine presence due to multiple stressors and degenerative Lewis Bodies formation respectively. Dopamine also is found to stimulate BDNF (Brain-Derived Neurotrophic Factor) which plays the utmost important role in preventing Alzheimer’s and other degenerative cognitive diseases among the elderly. With dopamine and its myriads of positive effects resulting the mind and body in a state of calm and relaxed manner, an individual is at peace with himself and surroundings in the Godly presence, ready for submission and acceptance no matter what the worldly conditions are, as evidenced in the Hadith and Quranic verses below:
The nearest a servant comes to his Lord is when he is prostrating himself, so make supplication (in this state). [Sahih Muslim, Book of Prayer, Hadith: 482]
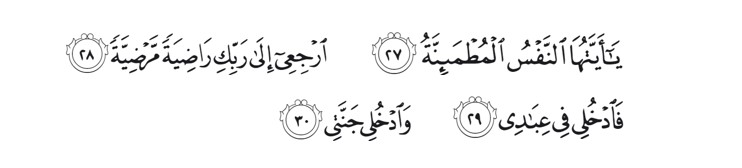
[To the righteous it will be said], "O reassured soul! Return to your Lord, well-pleased and pleasing [to Him], and enter among My [righteous] servants and enter My Paradise."
{Al-Fajr (The Dawn); verses 27-30}
Aidun mubarak. Minnal Aidil wal Faizin. Taqabbalallahu minna wa minkum.
BY:
Dr. Mohd Khairul Azizi Bin Mohd Zaki, MBBS (IIUM), IOC Dip Sp Phy (Lausanne)
Dr. Hazwani Binti Ahmad Yusof @ Hanafi, BSc. (UKM), MSc. (USM), PhD (Sydney)
[Lifestyle Science Cluster, Advanced Medical and Dental Institute, Universiti Sains Malaysia, Bertam, 13200 Kepala Batas, Pulau Pinang]
Chronic respiratory diseases (CRDs) are diseases of the airways and other structures of the lungs as defined by the World Health Organization (WHO). In addition to tobacco smoking as the commonest aetiology, other risk factors for CRDs include aerosol-based environmental origin irritants like air pollution, occupational chemicals and dust, and frequent childhood respiratory infections. CRDs can subsequently be grouped into 4 major categories (Prezant et al., 2008):
I. Upper respiratory tract disease: Chronic rhinosinusitis and reactive upper airways dysfunction syndrome
II. Lower respiratory tract diseases: Reactive lower airways dysfunction syndrome, irritant-induced asthma, and chronic obstructive airways diseases (COAD/COPD)
III. Parenchymal or interstitial lung diseases: Sarcoidosis, pulmonary fibrosis, and bronchiolitis obliterans
IV. Cancers of the lung and pleura
The commonly occurred interchangeably among all 4 are lower respiratory tract and parenchymal lung diseases, or better known as obstructive and restrictive lung disorders with regards to their pathogenesis nature despite their almost similarities in pathophysiology. Hence, diagnosing them requires a lung function test to differentiate one another. Obstructive lung disorders are mainly bronchial asthma (BA) and chronic obstructive pulmonary disease (COPD), which later can be subdivided into chronic bronchitis “Blue Bloaters” and emphysema “Pink Puffers”. Whereas, restrictive lung disorders are interstitial lung disease, pneumoconiosis and sarcoidosis. Lung cancer and tuberculosis can be considered as restrictive in nature albeit the mixed picture presentation in diagnostic laboratory findings.
Restrictive Lung Diseases
People with
restrictive lung disease cannot fully fill their lungs with air. Their lungs
are restricted from fully expanding. In contrast to obstructive lung disease
which is characterized by swollen airway (thickening of the respiratory wall)
leading to bronchoconstriction (narrowing of respiratory passage) with
excessive production of mucus (stimulating chronic irritative bouts of
coughing) due to ongoing prolonged inflammation process, restrictive lung
disease is due to stiffening of chest wall tissue, weakened muscles or even
damaged respiratory nerves resulting difficulty in fully expanding the lungs,
thus more difficult to fill the lungs with enough air for respiration purpose
as demanded by the body. In short, obstructive lung disease is
a “clogged/narrowed” condition, whilst the restrictive type is
a “tight/stiffened” condition. Here are the examples of this type of
respiratory illness (Isa, 2020);
a) Interstitial lung disease: Idiopathic Lung Fibrosis (scarring of alveolar tissue).
b) Pneumoconiosis: Occupational dust; asbestos (Asbestosis) and silica (Silicosis).
c) Sarcoidosis: Autoimmune granulomas altering multiple organs’ structure and function.
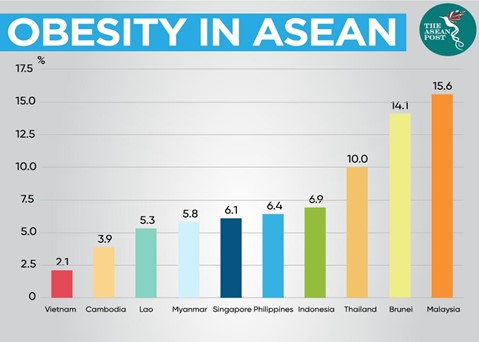
d) Obesity: Obesity Hypoventilation Syndrome
e) Scoliosis: Abnormal “S”-shaped curvature of spine, resulting depressed chest wall shape.
f) Neuromuscular diseases:
g) Childhood muscular dystrophy (Duchenne and Becker)
h) Adulthood progressive motor neurons breakdown (Amyotrophic Lateral Sclerosis/ALS)
Lung function tests like spirometry
and peak flow meter are the ones able to diagnose a patient with the symptom of
exertional shortness of breath to be whether obstructive or restrictive in
nature. It is based on the parameters of Forced Vital Capacity/FVC (volume of
air forcibly blown out after a full inspiration) and Forced Expiratory
Volume/FEV1 (amount of air exhaled from the lungs in the first 1 second after
full inspiration). A low FEV suggestive of obstructive lung disease, on the
other hand, an addition of low FVC signifies restrictive lung disease.
Lung Cancer
Squamous Cell
Carcinoma (SCC) is the commonest type of lung malignancy, however,
Adenocarcinoma is trending in recent years. SCC is associated with male and
smoking prevalence, while Adenocarcinoma type is linked to female and
non-smoking populations. It is postulated that this fact is due to secondary
smoking (passive smoker) ‘culture’ existing at large within our very own
society. All together, any types of cancer are almost always in a linear
relationship with aging as evidenced through a Malaysian study (Liam et al.,
2006) stating the age of peak incidence of lung cancer is 7th decade
of life.
At clinical
stages I and II, patients are able to undergo curative surgical resection of the
tumor site of the lungs. Inductive therapy, in the form of chemotherapy or in
combination with radiotherapy, is applied to stages III and IV patients in
order to downstage the lung malignancy prior to curative surgical resection if
feasible based on the treating pulmonologist’s (respiratory physician) judgment
in agreement with cardiothoracic surgeon’s further evaluation.
Tuberculosis
Tuberculosis
is a chronic lung infection caused by Mycobacterium tuberculosis.
The mode of spread among humans is via aerosol droplet transmission hence the
lungs are often the focus of tuberculous disease although TB may present with the
disease in any organ system (Chakrabarti et al., 2007). In Malaysia, it is more
prevalent among the foreign labor workers and in deeply rural regions due to
incomplete as well as inaccessibility to BCG (Bacillus Calmette–Guérin)
vaccination program. Recent years of vaccine hesitancy movements worldwide
might just hamper the efforts done to eradicate this once contagiously fatal
illness. A cross-sectional study by Amaral et al. (2015) using data collected
from across the globe, concluded that tuberculosis is associated with a mixed
presentation of airflow obstruction and restrictive patterns on spirometry
assessment.
Exercise Testing for Pulmonary Disease
Submaximal
graded exercise test (GXT) is used to assess cardiopulmonary function and
fitness by providing an objective measure of exercise capacity, mechanisms of
exercise intolerance, prognosis, and disease progression and treatment
response. Modifications of traditional protocols depend on functional
limitations and the onset of dyspnea. Test duration of 8–12 min is optimal for
those with mild-to-moderate illness (Buchfuhrer et al., 1983), whereas a test
duration of 5–9 min is recommended for patients with severe and very severe
disease (Benzo et al., 2007). SpO2 monitoring must be done for these
patients as they may exhibit oxyhemoglobin desaturation with exercise, with the
maintenance of SpO2 > 90% is recommended.
However, individuals with pulmonary disease may have ventilatory limitations to exercise. Thus, prediction of VO2peak based on age-predicted HRmax may not be appropriate as criteria for terminating the submaximal GXT. The 6-minute walking test (6MWT) and shuttle walking test can assess functional exercise capacity in individuals with more severe pulmonary disease and in settings that lack exercise testing equipment. The use of bronchodilator therapy as a standby emergency medication is beneficial for such individuals. Exertional dyspnea is a common symptom in people with any pulmonary disease. The modified Borg Category-Ratio 0–10 (CR10) Scale (Figure 1) has been used extensively to measure dyspnea before, during, and after exercise (Ries, 2006). Patients should be given specific, standardized instructions on how to relate the wording on the scale to their level of breathlessness. In addition to standard termination criteria, exercise testing may be terminated because of severe arterial oxyhemoglobin desaturation. The exercise testing mode is walking or stationary cycling. Walking protocols may be more suitable for individuals with severe diseases who lack the muscle strength to overcome the increasing resistance of cycle leg ergometers. Arm ergometry may result in increased dyspnea that may limit the intensity and duration of the activity.
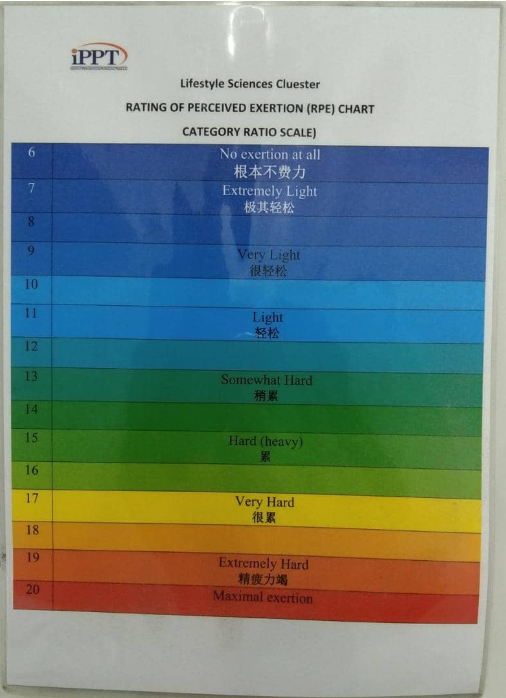
Figure 1: Modified Borg CR10 Scale for Dyspnea
Photo by IPPT
Exercise Prescription
Despite
substantially less investigation into the benefits of exercise training in
non-obstructive chronic lung diseases, strong scientific evidence supports the
inclusion of exercise training for many lung diseases other than Bronchial
Asthma and COPD with demonstrated clinical and physiologic benefits (Rochester
et al., 2014). However, the exercise programs should be modified to include
disease-specific strategies. Methods for adapting exercise training in patients
with restrictive chronic lung disease have been published (Holland et al.,
2013). Exercise training recommendations have been specifically presented for
patients with stable interstitial lung disease who are receiving optimal
medical management. For these patients, the FITT guidelines as below:
F: 3-5
day/week
I: Moderate
intensity. Intensities should be below those that would provoke severe dyspnea,
oxygen desaturation, or in some cases, hypertensive episode due to chronic
illness.
T: Morning
T: Aerobic
exercise should comprise the core component of the exercise program. Resistance
exercise training may be added after the aerobic training is established and
well tolerated.
Precautions:
Arm ergometry,
heavy resistance training, and pelvic floor exercise should be avoided to
reduce the risk of a Valsalva maneuver.
Apart from the
standard ACSM guideline meant for COPD, according to a local guideline by
National Cancer Society Malaysia (NCSM) issued in 2019; seated exercises are
the best form of training for lung cancer patient to build strength and
endurance, eliminating the risk of difficulty in breathing; with inhalation
during motion and exhalation when completing. This simple exercise steps can be
used for other restrictive lung diseases and tuberculosis patients as well, due
to its efficacy and safety with minimal effort without much exertion. The
seated exercise consists of:
1. Leg lift (alternating lift legs up to shoulders while sitting on a chair for 10 times)

Figure 2: Leg Lifts
Photo by Dr. Azizi
2. Seated kicks (kick foot off floor while sitting on a chair for 10 times)

Figure 3: Seated Kicks
Photo by Dr. Azizi
3. Overhead arm lifts (lift arms towards ceiling while sitting on a chair for 10 times)

Figure 4: Overhead Arm Lifts
Photo by Dr. Azizi
4. Windmills (circling arms while sitting on a chair for 10 times)

Figure 5: Windmills
Photo by Dr. Azizi
5. Pursed lip breathing is a good method to ‘retrain’ breathing regulation for lung cancer patients, simply by breath in through nostrils and slowly breath out through mouth by pursing the lips (like “blowing the candle” or “pulling out a thread from mouth”).
6. Buteyko breathing technique; a
nasal breathing (inhaling and exhaling via the nostrils) method; can be applied
as the exercise progresses, to control and prevent hyperventilation episodes
caused by the pulmonary diseases.
Special
Considerations
Peripheral
muscle dysfunction in the case of neuromuscular diseases (eg., Duchenne/Becker
and ALS) contributes to exercise intolerance and is significantly and
independently related to increased use of health care resources, poorer
prognosis, and mortality. Maximizing pulmonary function using bronchodilators
before exercise training in those with airflow limitation can reduce dyspnea
and improve exercise tolerance (Spruit et al., 2013). Inspiratory muscle
weakness is a contributor to exercise intolerance and dyspnea in those with
chronic lung disease. In patients receiving optimal medical therapy who still
present with inspiratory muscle weakness and breathlessness, Inspiratory muscle
training (IMT) , despite no clear guidelines for it, may prove useful in those
unable to participate in exercise training with an intensity of the training
load of at least 30% of maximal inspiratory pressure has been recommended
(Langer et al., 2009). IMT improves inspiratory muscle strength and endurance,
functional capacity, dyspnea, and quality of life which may lead to
improvements in exercise tolerance (Gosselink et al., 2011). Supplemental
oxygen is indicated for patients with SpO2 < 88% while breathing room air
(Qaseem et al., 2011). This recommendation applies when considering
supplemental oxygen during exercise. In patients using ambulatory supplemental
oxygen, flow rates will likely need to be increased during exercise to maintain
SpO2 > 88%. Although inconclusive, there is evidence to suggest the
administration of supplemental oxygen to those who do not experience
exercise-induced hypoxemia may lead to greater gains in exercise endurance
particularly during high intensity exercise (Nonoyama et al., 2007).
Individuals suffering from acute exacerbations of their pulmonary disease
should limit exercise until symptoms have subsided.
1) Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower
respiratory diseases after occupational and environmental disasters. Mt Sinai J
Med. 2008 Mar-Apr;75(2):89-100. doi: 10.1002/msj.20028. PMID: 18500710.
2) Liam CK, Pang YK,
Leow CH, Shyamala P, Menon AA. Changes in the distribution of lung cancer cell
types and patient demography in a developing multiracial Asian country. Lung
Cancer 2006; 53:23-30.
3) Chakrabarti B, Calverley PM, Davies PD. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2007;2(3):263-72. PMID: 18229564; PMCID: PMC2695198.
4) Amaral AF, Coton S, Kato B, Tan WC, Studnicka M, Janson C, Gislason T, Mannino D, Bateman ED, Buist S, Burney PG; BOLD Collaborative Research Group. Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J. 2015 Oct;46(4):1104-12. doi: 10.1183/13993003.02325-2014. Epub 2015 Jun 25. PMID: 26113680; PMCID: PMC4594762.
5) Buchfuhrer MJ,
Hansen JE, Robinson TE, Sue DY, Wasserman K, Whipp BJ. Optimizing the exercise
protocol for cardiopulmonary assessment. J Appl Physiol Respir Environ Exerc
Physiol. 1983;55(5):1558–64.
6) Benzo RP,
Paramesh S, Patel SA, Slivka WA, Sciurba FC. Optimal protocol selection for
cardiopulmonary exercise testing in severe COPD. Chest. 2007;132(5):1500–5.
7) Ries AL. Impact
of chronic obstructive pulmonary disease on quality of life: the role of
dyspnea. Am J Med. 2006;119(10 Suppl 1):12–20.
8) Rochester CL, Fairburn
C, Crouch RH. Pulmonary rehabilitation for respiratory disorders other than
chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(2):369–89.
9) Holland AE, Wadell K,
Spruit MA. How to adapt the pulmonary rehabilitation programme to patients with
chronic respiratory disease other than COPD. Eur Respir Rev.
2013;22(130):577–86.
10) National Cancer Society
Malaysia. 2019. Cancer & Physical Activity Booklet.
11) Spruit MA, Singh SJ, Garvey
C, et al. An official American Thoracic Society/European Respiratory Society
statement: key concepts and advances in pulmonary rehabilitation. Am J Respir
Care Med. 2013;188:e13–64.
12) Langer D, Hendriks E,
Burtin C, et al. A clinical practice guideline for physiotherapists treating
patients with chronic obstructive pulmonary disease based on a systematic
review of available evidence. Clin Rehabil. 2009;23(5):445–62.
13) Gosselink R, De Vos J, van
den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle
training in patients with COPD: what is the evidence? Eur Respir J.
2011;37(2):416–25.
14) Qaseem A, Wilt TJ,
Weinberger SE, et al. Diagnosis and management of stable chronic obstructive
pulmonary disease: a clinical practice guideline update from the American
College of Physicians, American College of Chest Physicians, American Thoracic
Society, and European Respiratory Society. Ann Intern Med. 2011;155:179–91.
15) Nonoyama M, Brooks D,
Lacasse Y, Guyatt GH, Goldstein RS. Oxygen therapy during exercise training in
chronic obstructive pulmonary disease. Cochrane Database Syst Rev.
2007;(2):CD005372.
Author(s):
Dr. Mohd Khairul Azizi Bin Mohd Zaki, MBBS (IIUM), IOC
Dip Sp Phy (Lausanne)
Dr.
Hazwani Binti Ahmad Yusof @ Hanafi, BSc. (UKM), MSc. (USM), PhD (Sydney)
MSc Clinical Exercise Science
(TCE508: Exercise Programming for Clinical Populations)
Lifestyle Science Cluster
AMDI, USM
.png)



Menurut Kamus Dewan Bahasa dan Pustaka, perkataan
“gembira” bermaksud sangat suka, sangat girang dan besar hati. Mempunyai
perasaan gembira adalah salah satu sifat semulajadi manusia. Terdapat pelbagai
perkara dan cara yang boleh membuatkan anda merasai gembira dalam hidup. Semudah
senyum pada diri sendiri atau sesama individu lain, melakukan hobi yang disukai,
bersama dengan insan yang disayangi serta meluangkan masa bercuti di tempat-tempat
peranginan dapat melahirkan rasa gembira dalam sanubari secara zahiriah mahupun
batiniah. Selain itu, senaman juga turut mampu memberikan kegembiraan kepada
seseorang samada dilakukan secara individu ataupun berkumpulan. Apakah
mekanisma di sebalik senaman yang membolehkan insan itu berasa gembira?
D.O.S.E. (Sains Sukan)
Melakukan aktiviti fizikal samada bersenam dan
juga bersukan banyak mendorong seseorang itu menjadi lebih gembira dari biasa. Ia
dihasilkan melalui proses fisiologi tubuh manusia secara semulajadi dengan meningkatkan
kadar rembesan hormon-hormon gembira (happy hormones) dalam badan melalui isyarat
dihantar ke/dari otak. “Happy hormones” yang terbabit adalah seperti berikut;
Dopamine: ‘hormon ganjaran’ (Reward Hormone)
Oxytocin: ‘hormon cinta’ (Love Hormone)
Serotonin: ‘hormon ketenangan’ (Calm Hormone)
Endorphin: ‘hormon keazaman’ (Willpower Hormone)
Dopamine berfungsi dalam ‘Sistem Ganjaran’
badan manusia yakni membuatkan individu tersebut berasa seronok dan puas dengan
apa yang diidami/diingini. Hormon inilah yang terlibat secara langsung dalam
ketagihan/motivasi terhadap sesuatu perbuatan (hobi/pekerjaan) atau bahan
(makanan/minuman khas, rokok, dadah). Oxytocin pula mempengaruhi penguncupan rahim
ketika bersalin dan penyusuan badan bagi wanita khasnya. Ia bertindak melalui
rangsangan seksual yang melibatkan hubungan kasih sayang antara dua insan yang
bercinta atau kasih seorang ibu terhadap anaknya. Manakala, Serotonin berperanan sebagai penstabil
emosi serta memantapkan proses pembelajaran dan daya ingatan/memori. Endorphin
ataupun “Endogenous Morphine” bertindak sebagai penghalang isyarat kesakitan
dan menaikkan rasa ‘euphoria’ (keseronokan yang tak terhingga), malah dikenali
sebagai “runner’s high” atau “rower’s high” bagi sukan acara larian jarak jauh
(lebih 400m) dan rowing. Kesemua hormon ini akan meningkat parasnya (terutama
sekali, Endorphin) selari dengan peningkatan intensiti dan kekerapan melakukan
sesuatu aktiviti olahraga. Senaman berbentuk HIIT (High Intensity Interval Training) yang semakin popular dalam kalangan masyarakat adalah contoh aktiviti olahraga "quick fix" yang mudah dilakukan oleh sesiapa sahaja untuk meningkatkan paras hormon-hormon D.O.S.E. ini.
D.O.S.E. (Perubatan Klinikal)
Hormon-hormon yang dinyatakan juga dihasilkan
secara sintetik/tiruan bagi tujuan rawatan mengikut keperluan dan penyakit yang
dihadapi. Semua hormone tersebut mempunyai peranan berbeza sebagai ubat-ubatan
dari bidang perubatan yang berlainan kepakaran bagi menangani kondisi pesakit
yang berbeza serta penyakit di sebaliknya.
D = Levodopa (Parkinson's disease) - Neurologi
O = Pitocin 5 IU (induksi bersalin), 10 IU (pendarahan rahim selepas
bersalin) - O&G (Perbidanan)
S = Escitalopram, Fluoxetine, Sertraline (Depression/Kemurungan dan
Anxiety/Keresahan) - Psikiatri
E = Oxycodone/Hydrocodone/Codeine, Fentanyl, Morphine (tahan sakit) – Anaesthesiologi
Levodopa adalah ubat yang digunakan untuk
merawat penyakit Parkinson’s. Parkinson’s disease terjadi apabila penghasilan hormone
Dopamine secara semulajadi berkurangan akibat daripada kematian sel-sel neuron
di bahagian Substantia Nigra dalam otak, yang disebabkan oleh proses penuaan
dan juga sejarah kecederaan berkali-kali di kepala (sebagai contoh; arwah Muhammad
Ali, lagenda tinju dunia). Pitocin digunakan oleh doktor berkepakaran obstetrik
(perbidanan) dalam dua keadaan beserta dua dos yang berbeza. Jika kandungan
sudah matang (38-40 minggu tempoh gestasi) tetapi tiada tanda-tanda kelahiran
(pecah air ketuban, kontraksi rahim dan “show” campuran lendir-darah rahim),
Pitocin 5 IU akan dicampur dengan 450mL Normal Saline dan disalurkan secara
intravenous (melalui saluran darah pesakit) beserta tinjauan berkala oleh jururawat
perbidanan yang bertugas untuk mempercepatkan (induksi) proses kelahiran. Andai
berlaku pendarahan yang teruk sejurus lepas bersalin, Pitocin 10 IU pula dicampur
dengan 450mL Normal Saline dan juga disalurkan secara intravenous dengan laju
bagi membolehkan rahim mengeras kembali selepas bersalin. Pendarahan selepas
bersalin (Postpartum Haemorrhage) ditentukan berdasarkan kuantiti darah terkumpul
pada perkakas ‘Kidney Dish’ digunakan; satu yang penuh (500mL) bagi bersalin secara
normal (Spontaneous Vertex Delivery/SVD) dan dua yang penuh (1000mL) bagi yang menjalani
pembedahan Caesarean Section (C-Sec). Ubat ‘Selective Serotonin Reuptake Inhibitors’
(SSRIs) berfungsi meningkatkan Serotonin dalam darah dengan menghalang hormon
tersebut diambil kembali oleh ‘presynaptic cells’. Antara contoh SSRIs ialah
Escitalopram, Fluoxetine dan Sertraline yang banyak digunakan oleh doktor pakar
sakit mental (psikiatrik), bagi menangani masalah kemurungan (Major Depressive
Disorder) dan keresahan (Generalized Anxiety Disorder, Panic Disorder, Phobias,
Obsessive-Compulsive Disorder). Oxycodone/Hydrocodone/Codeine, Fentanyl dan
Morphine merupakan ubat-ubatan dari kelas 'Opiods' yang seringkali digunakan oleh
doktor pakar anaesthesiologi untuk menahan/menghilangkan rasa sakit pada pesakit, terutama
sekali tatkala melakukan sesuatu pembedahan yang besar atau mengalami kesakitan yang teruk dan berpanjangan (chronic pain) disebabkan oleh kanser atau osteoarthritis (keradangan tulang dan sendi).
Kesimpulannya, hormon D.O.S.E. berperanan amat penting dalam hidup semua insan. Perasaan gembira itu sahaja dapat membuatkan individu tersebut rasa bersemangat untuk meneruskan amalan kehidupan seharian. Setiap D.O.S.E. mempunyai proses serta tugas tersendiri yang terbukti melalui penggunaan hormon tersebut secara sintetik dalam bidang perubatan untuk menyelamatkan nyawa pesakit dan menambahbaikkan kondisi fizikal serta mental yang bergelumang dengan kemurungan atau keresahan akibat krisis hidup iaitu tekanan, penuaan dan juga kecederaan. Aktiviti fizikal samada senaman dan juga bersukan terbukti meningkatkan paras hormon D.O.S.E. jika lebih kerap dilakukan dan juga apabila dilaksanakan pada intensiti yang tinggi. Justeru, D.O.S.E. boleh memberi perlindungan semulajadi kepada tubuh manusia sebagai persiapan menghadapi krisis kehidupan yang bakal dihadapi seperti dinyatakan sebelum ini, dengan hadirnya rasa gembira seterusnya menambahbaikkan kualiti kehidupan individu tersebut serta memelihara kemandirian spesies sejagat.
Nukilan oleh:
Dr. Mohd Khairul Azizi Bin Mohd Zaki
MBBS (IIUM), IOC Dip Sp Phy (Lausanne)
Kluster Sains Gaya Hidup, IPPT USM

Nur Syamimi Anisah Binti Saharudin, Hafizuddin Mohamed Fauzi
Kluster Prerubatan Regeneratif, Institut Perubatan dan Pergigian Termaju, Universiti Sains Malaysia.
Pengenalan
Sifilis adalah penyakit kelamin berjangkit dan mampu mengancam nyawa. Ia berpunca daripada sejenis bakteria iaitu Treponema pallidum. Penularan jangkitan sifilis membabitkan manusia ke manusia boleh berlaku melalui kongenital ( kelahiran) dan ‘acquired’ iaitu melalui sentuhan kulit.
Dikenali sebagai penyakit global, terdapat sebanyak 11 juta kes jangkitan sifilis didaftarkan kepada World Health Organization (WHO) pada setiap tahun. Pada tahun 2012 sahaja, sebanyak 5.6 Juta kes telah dilaporkan dari seluruh dunia. Manakala, mengikut laporan yang dikeluarkan oleh Kementerian Kesihatan Malaysia (KKM), peningkatan kes telah berlaku sebanyak 6.7% sejak tahun 2006 di Malaysia. Untuk itu kesedaran di kalangan masyarakat amat penting bagi mencegah pertambahan kes.
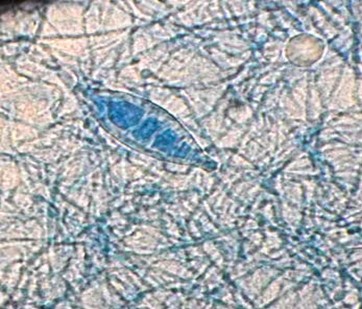
Etiologi
T.pallidum adalah sejenis bakteria sub-spesies spiroket yang bersifat patogenik terhadap tubuh badan manusia. Ianya berbentuk spiral, berstruktur tirus di hujung tubuh dan mempunyai filamen untuk bergerak aktif. Namun, T.pallidum merupakan bakteria yang tidak dapat hidup diluar hos dan tidak mampu bertahan pada suhu bilik dan memerlukan hos seperti manusia atau haiwan.
Jangkitan sifilis
Ia merebak melalui sentuhan rapat kulit ke kulit melalui hubungan kelamin dan oral seks. Dengan bermula dari luka kecil, ia akan memasuki saluran darah lalu merebak ke kelenjar limfa dan menyebabkan keradangan saluran arteri yang memusnahkan tisu badan.
Peringkat jangkitan sifilis dikategorikan mengikut tahap keseriusan dan jangkamasa tempoh jangkitan.‘Acquired syphilis’ terdiri daripada dua tahap iaitu sifilis awal dan sifilis lewat.
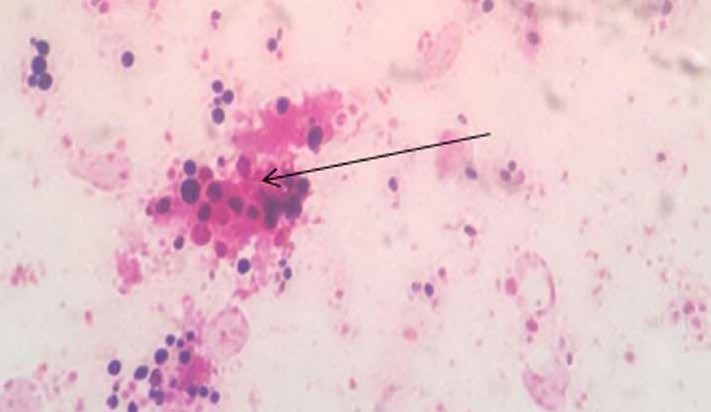
Sifilis awal
Bagi jangkitan sifilis yang dihidapi dalam masa kurang dua tahun akan dibahagikan kepada tiga peringkat iaitu peringkat primer, sekunder dan tertiar atau laten awal. Gejala utama dalam peringkat primer adalah ulser atau ‘chancre’ yang boleh didapati selepas 18 hingga 21 hari jangkitan. Ia bermula dengan kehadiran papul (bintat kecil yang keras) yang berubah menjadi ulser dan berakhir sebagai ‘chancre’ iaitu luka tanpa nanah dan tidak rasa sakit. Chancre’ ini berpotensi tinggi untuk dijangkiti tetapi akan hilang dengan sendiri dalam tempoh 1-6 minggu. Simptom lain sewaktu ‘acquired syphilis’ adalah demam, sakit kepala, turun berat badan, rambut gugur, bengkak limfa dan penyakit meningitis. Sifilis sekunder berlaku sekiranya sifilis primer tidak dirawat dengan kehadiran simptom-simptom tambahan seperti ruam dikulit, ketumbuhan ketuat yang tumbuh pada kulit dan bengkak kelenjar limfa.

Figur 1 : Ulser peringkat primer

Figur 2: Ruam di tapak tangan peringkat sekunder
Sifilis Lewat
Pada fasa ini, bakteria berada dalam keadaan dorman sekaligus berupaya untuk merosakkan tubuh badan secara perlahan-lahan tanpa sebarang gejala. Jika tidak dirawat is akan menyebabkan kerosakkan jantung, otak, tulang dan sistem saraf. Ini boleh mambawa maut.
Sifilis kongenital
Jangkitan ini melibatkan ibu dan anak di dalam kandungan. Meskipun begitu, bayi tidak akan menunjukkan simptom sebaik dilahirkan malahan ianya boleh mengambil masa sehingga beberapa minggu, bulan atau tahun selepas kelahiran. Jangkitan ini terbahagi kepada dua peringkat iaitu jangkitan awal dengan simptom ruam, selsema berdarah, bengkak limfa, kecacatan tulang, kerosakan sistem saraf dan gangguan penglihatan. Peringkat akhir akan mengakibatkan inflamasi yang kronik, cacat hidung, pekak, masalah kognitif dan sendi.
Diagnosis
Terdapat dua jenis ujian iaitu ujian saringan dan pengesahan.
a) Ujian saringan
Berfungsi sebagai penunjuk sama ada seseorang itu dijangkiti atau tidak. Terdapat dua jenis ujian saringan:
• Venereal Disease Research Laboratory test for syphilis (VDRL)
• Rapid Plasma Reagin (RPR).
Keputusan ujian positif VDRL dan RPR dinilai daripada kekuatan gumpalan yang terhasil. Jika kekuatan gumpalan itu dalam nisbah 1:8, ia adalah positif. Gambar 1 merupakan contoh hasil ujian kit RPR.
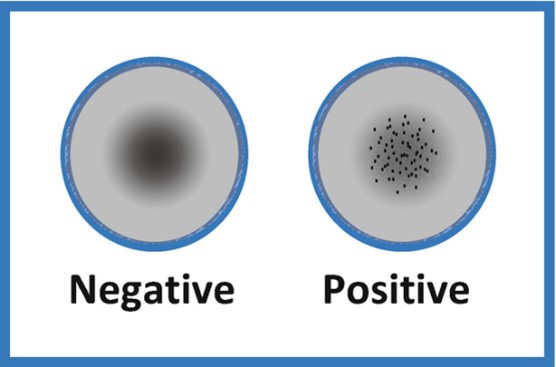
Figur 3: Ujian kit RPR. Dari kiri, keputusan negatif kerana tiada gumpalan terhasil. Dari kanan, keputusan positif dengan gumpalan terhasil.
Ujian ini bukan ujian pengesahan kerana ia boleh memberikan keputusan positif palsu dalam kes kes seperti:
• Hamil
• Penyakit autoimun
• Ahli bina badan.
b) Ujian pengesahan
Ujian ini dijalankan selepas keputusan positif diperoleh dari ujian saringan. Contoh ujian adalah seperti:
• Treponema pallidum particle agglutination (TPPA)
• Treponema pallidum hemagglutination (TPPHA)
• Ujian serologi Anti-T.Palidum IgM antibodi spesifik.
Keputusan positif palsu juga mungkin dapat diperoleh dari kes-kes tertentu seperti systemic lupus erythematous (SLE) dan Lyme disease dan untuk itu ia harus di tafsirkan berdasarkan sejarah klinikal oleh doktor yang merawat.
Rawatan
Sifilis dapat dirawat dengan ubat anti-bakteria ( antibiotic ). Namun, ia bergantung kepada tahap jangkitan. Rawatan, antibiotik akan diberikan secara suntikan atau pil dengan dos tertentu mengikut peringkat jangkitan. Jenis antibiotik yang akan diberikan adalah seperti di dalam jadual 1:
?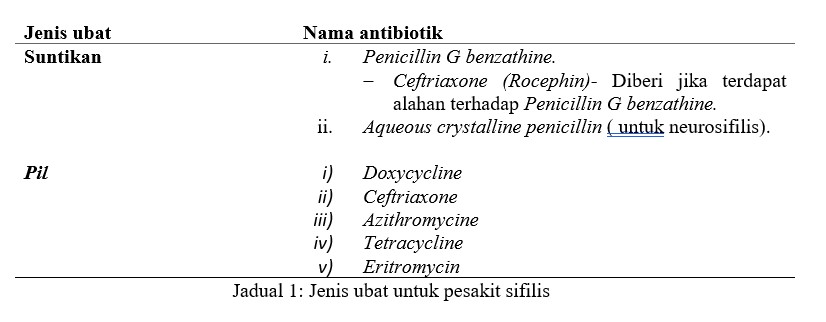
Keadaan fizikal dan gejala pesakit perlu sentiasa diawasi dan ujian makmal ulangan perlu dijalankan dalam tempoh 6 dan 12 bulan bagi tujuan penilaian terhadap keberkesanan rawatan yang diterima.
Konklusi
Walaupun penyakit sifilis ini berisiko tinggi dan boleh membawa maut, ia boleh dirawat jika dapat dikesan secara awal. Oleh itu, amat penting untuk anda kenali gejala awal jangkitan dan terus menjalani ujian saringan jika anda mempunyai risiko jangkitan terutamanya kepada individu yang sering melakukan hubungan seks bebas.
Rujukan
1. Organization, W. H. (2016). WHO guidelines for the Treatment of Treponema Pallidum (Syphilis). Geneva: WHO Document Production Services, Geneva, Switzerland.
2. Syphilis. Retrieved September, 2020, from www.cdc.gov/nchstp/dstd/Stats_Trends/1999Surveillance/99pdf/99Section4.pdf.
3. Alhabbab R.Y. (2018) Treponema pallidum Hemagglutination (TPHA) Test. In: Basic Serological Testing. Techniques in Life Science and Biomedicine for the Non-Expert. Springer, Cham. https://doi.org/10.1007/978-3-319-77694-1_5
4. syphilis. Retrieved September, 2020 from www.niaid.nih.gov/factsheets/stdsyph.htm.
5. Treponema pallidum. Retrieved September 2020, from https://www.slideshare.net/Prbn/treponema-pallidum-49670354
6. WHO. Sexually Transmitted Infections Factsheet. August 2016. Availablefrom:http://www.who.int/mediacentre/factsheets/fs110/en/ Accessed September 2020.
7. Pressreader. Punca jangkitan penyakit kelamin meningkat. 2017. Accessed on October 2020. Available from: https://www.pressreader.com/malaysia/berita-harian malaysia/20171204/2817326798123391998;16:699-711,xi.









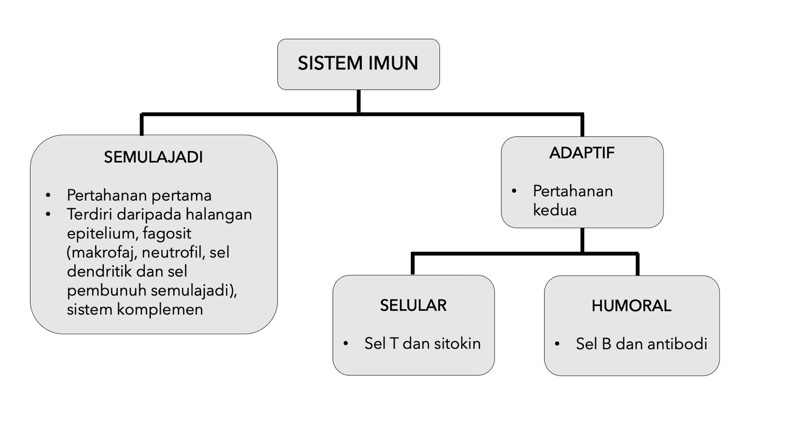






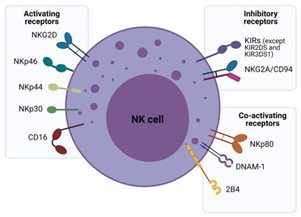
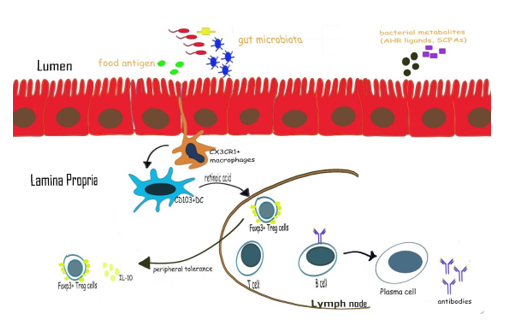
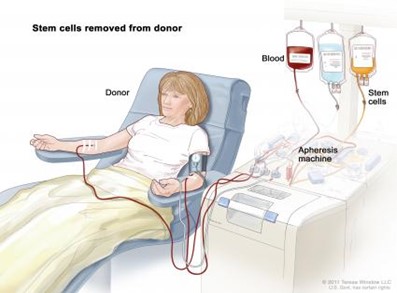
 Kedua-dua sitokin ini penting untuk mengaktifkan dan membiak sel T sitotoksik atau sel T CD8+. Sebagai alternatif, molekul MHC-I pada APC yang terikat pada sel T CD8+ dan menjana set T sitotoksik khusus antigen dengan kehadiran sitokin sel T pembantu 1 (Th1), IL-2 dan
Kedua-dua sitokin ini penting untuk mengaktifkan dan membiak sel T sitotoksik atau sel T CD8+. Sebagai alternatif, molekul MHC-I pada APC yang terikat pada sel T CD8+ dan menjana set T sitotoksik khusus antigen dengan kehadiran sitokin sel T pembantu 1 (Th1), IL-2 dan  Di samping itu, molekul MHC-II pada APC mengikat dengan sel T pembantu 2 (Th2) yang merangsang rembesan IL-4 dan IL-10 serta berinteraksi dengan sel B untuk menggalakkan pengeluaran antibodi khusus antigen. Sebaliknya, sel NK secara khusus mengecam molekul MHC-I yang dinyatakan oleh sel normal, dan pengecaman ini menghalang sel NK membunuh sel normal. Jika molekul MHC-I pada sel normal diubah atau tidak hadir kerana jangkitan atau transformasi virus, isyarat perencatan akan berkurangan yang akan meransang aktiviti sitotoksik terhadap sel sasaran [4]. Induksi sel NK adalah pilihan terapeutik tambahan dalam terapi peningkatan imun angkat (AIET). Sel NK dan DC saling bertindak balas antara satu sama lain. Maksudnya, sel DC yang diaktifkan akan mencetuskan aktiviti sel NK dan induksi tindak balas anti-tumor. Secara timbal balik, sel NK juga mengaktifkan sel DC, meningkatkan keupayaan mereka untuk menghasilkan sitokin pro-tumor dan merangsang tindak balas imun pengantara sel T (CD4+ dan CD8+) [5,6]. Ringkasan tindak balas sel-sel imun yang terlibat dalam kaedah terapi peningkatan imun angkat (AIET) terhadap sel-sel kanser diilustrasi dalam gambarajah 1.
Di samping itu, molekul MHC-II pada APC mengikat dengan sel T pembantu 2 (Th2) yang merangsang rembesan IL-4 dan IL-10 serta berinteraksi dengan sel B untuk menggalakkan pengeluaran antibodi khusus antigen. Sebaliknya, sel NK secara khusus mengecam molekul MHC-I yang dinyatakan oleh sel normal, dan pengecaman ini menghalang sel NK membunuh sel normal. Jika molekul MHC-I pada sel normal diubah atau tidak hadir kerana jangkitan atau transformasi virus, isyarat perencatan akan berkurangan yang akan meransang aktiviti sitotoksik terhadap sel sasaran [4]. Induksi sel NK adalah pilihan terapeutik tambahan dalam terapi peningkatan imun angkat (AIET). Sel NK dan DC saling bertindak balas antara satu sama lain. Maksudnya, sel DC yang diaktifkan akan mencetuskan aktiviti sel NK dan induksi tindak balas anti-tumor. Secara timbal balik, sel NK juga mengaktifkan sel DC, meningkatkan keupayaan mereka untuk menghasilkan sitokin pro-tumor dan merangsang tindak balas imun pengantara sel T (CD4+ dan CD8+) [5,6]. Ringkasan tindak balas sel-sel imun yang terlibat dalam kaedah terapi peningkatan imun angkat (AIET) terhadap sel-sel kanser diilustrasi dalam gambarajah 1.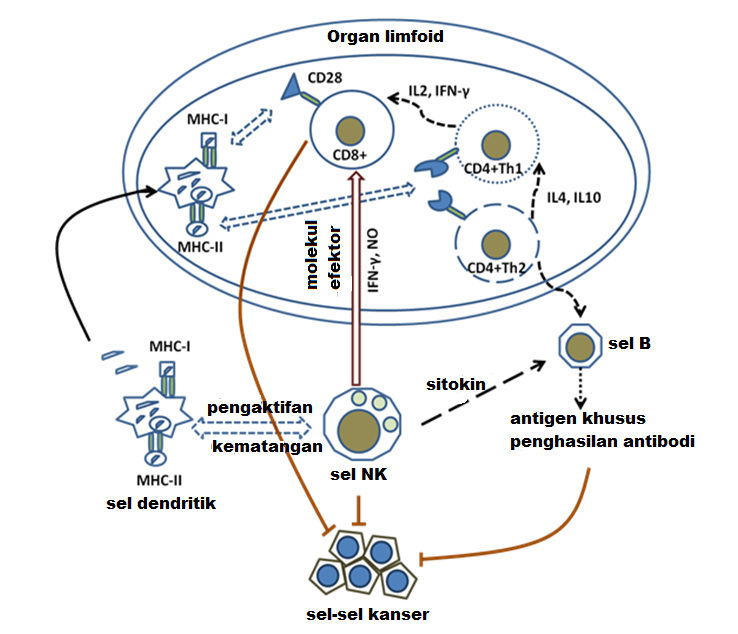


Prof Madya Dr Bakiah binti Shaharuddin
Pakar Oftalmologi, Kluster Perubatan Regeneratif, Institut Perubatan dan Pergigian Termaju, Universiti Sains Malaysia
Mata anda merah dan gatal - apa penyebabnya?
Alahan atau alergik mata (allergic conjunctivitis) adalah tindak balas imun tidak diingini yang berlaku apabila mata terdedah kepada bahan-bahan tertentu yang mengakibatkan gejala mata gatal, kemerahan atau tidak selesa. Bahan-bahan ini dipanggil alergen. Alergen adalah protein yang terdapat pada habuk, debunga, bulu haiwan, atau protin dalam makanan seperti kacang, telur, makanan laut, dan lain-lain yang boleh menimbulkan reaksi auto imun kepada sebahagian manusia.
Di antara gejala alahan mata adalah termasuk; mata gatal atau pedih, mata berair, mata merah, kulit kering dan bersisik atau kelopak mata bengkak. Gejala-gejala ini boleh terdapat pada satu mata atau kedua-dua belah mata.
Bagaimanakah alahan mata boleh dikesan?
Pakar mata mungkin merujuk anda kepada pakar alahan untuk menentukan diagnosis sebenar. Pakar alahan biasanya akan melakukan ujian tusukan kulit ‘skin prick test” untuk menentukan punca alahan anda. Sejumlah kecil alergen akan dicucuk masuk di bawah kulit untuk melihat sama ada ia merangsang tindak balas pada tempat tusukan. Benjolan merah dan bengkak adalah kesan tindak balas tersebut. Ini membantu pakar alahan mengenal pasti alergen yang anda paling sensitif.
Rawatan untuk alahan mata
Cara terbaik untuk merawat sebarang bentuk alahan adalah langkah-langkah pencegahan daripada terdedah kepada alergen. Langkah-langkah pencegahan termasuk mengawal diri dari makanan tertentu contohnya; tidak menggunakan karpet bagi mengurangkan habuk, kerap menukar cadar atau sarung bantal, membersihkan langsir atau ‘blinds’ dengan kerap, tidak memelihara haiwan seperti kucing atau burung, dan lain-lain langkah berdasarkan alergen yang berkaitan.
Sekiranya alahan mata terjadi, terdapat beberapa rawatan yang boleh melegakan gejala. Ubat-ubatan ini diambil samada secara oral, disembur ke dalam hidung atau ubat titisan mata.
Antara ubatan secara oral adalah; antihistamin seperti loratadine (Claritin) atau diphenhydramine (Benadryl), dekongestan seperti pseudoephedrine (Sudafed) atau oxymetazoline (Afrin) dan juga steroid seperti prednisolone dalam kes yang serius dan selepas diarahkan oleh doktor.
Ubat titisan mata yang kerap digunakan mengandungi antihistamin seperti olopatadine hydrochloride dengan jenama Pataday atau Patanol. Ubat lain mengandungi anti-radang bukan steroid (NSAIDs) seperti ketorolac (Acular, Acuvail). Manakala ubat steroid seperti Predforte atau Maxidex, dengan preskripsi doktor. Air mata tiruan juga boleh membantu. Sesetengah ubat titisan mata mesti digunakan setiap hari, manakala yang lain boleh digunakan mengikut keperluan untuk melegakan gejala.
Selain alahan, mata merah dan gatal juga mungkin disebabkan oleh keadaan lain seperti jangkitan, mata kering atau keradangan. Satu cara untuk mengetahui sama ada anda menghadapi alahan berbanding dengan jangkitan mata, ialah anda akan mengalami reaksi alahan lain, seperti bersin, hidung tersumbat (rhinitis) atau kulit yang gatal dan bersisik (eczema). Sebahagian besar pesakit yang mempunyai alahan mata juga merupakan pesakit asthma (lelah).
Pesanan Akhir
Jika anda mempunyai alahan, anda mungkin akan mengalami gejala alahan mata apabila terdedah kepada alergen tertentu. Walaupun tiada ubat untuk alahan, rawatan boleh membantu melegakan gejala yang tidak menyenangkan dan mengelakkan dari komplikasi yang lebih serius. Ubat-ubatan oral, semburan dan titisan mata adalah berkesan dalam kebanyakan kes. Dapatkan nasihat dari doktor bagi rawatan yang selamat dan optima.
Penulis Artikel
Prof Madya Dr Bakiah binti Shaharuddin
Pakar Oftalmologi, Institut Perubatan dan Pergigian Termaju, USM







Dr Nor Hazwani Ahmad
Kluster Sains Onkologi Dan Radiologi, Institut Perubatan dan Pergigian Termaju (IPPT), USM
Artemisinin telah ditemui pada tahun 1971
dan merupakan sebatian yang diperoleh daripada tumbuhan Artemisia annua.
Artemisinin telah disyorkan oleh Organisasi Kesihatan Sedunia dalam kombinasi
dengan ubat antimalaria lain untuk merawat strain rintang dadah Plasmodium
falciparum, malaria serebrum dan malaria di kalangan kanak-kanak. Dalam
usaha untuk meningkatkan bioavailabiliti dan keberkesanan artemisinin, beberapa
derivatif telah disintesis seperti dihydroartemisin iaitu laktol terkurang yang
lebih aktif tetapi kurang stabil dari segi haba berbanding artemisinin; dan artesunat
yang lebih aktif dan kurang toksik daripada artemisinin. Semua terbitan ini
tergolong dalam keluarga besar sebatian artemisinin atau terbitan seperti
artemisinin yang berkongsi jambatan endoperoksida dan mengekalkan sebahagian
daripada sifat farmakologi artemisinin. Berdasarkan aktiviti sitotoksik mereka
terhadap Plasmodium falciparum, artemisinin dan derivatif separa
sintetiknya telah menunjukkan hasil yang memberangsangkan apabila dikaji secara
in vitro sebagai ubat antikanser dan antivirus.
Dalam beberapa kajian yang telah dijalankan,
artemisinin telah terbukti dapat menukar sel kanser yang tahan kepada sel
kanser yang sensitif, istilah yang dipanggil kemosensitisasi. Satu kajian telah
mendapati bahawa artemisinin, artesunat dan dihydroartemisinin, apabila
digabungkan dengan doxorubicin dan pirarubicin, dapat meningkatkan
sitotoksisiti mereka terhadap titisan sel leukemia K562/ADR P-glycoprotein-overexpressing,
dan titisan sel kanser paru-paru sel kecil GLC4/ADR MRP1-overexpressing.
Sesetengah derivatif artemisinin juga telah terbukti dapat menghalang P-glycoprotein
dalam sawar darah otak (blood brain barrier), dan menunjukkan ia berpotensi
untuk terapi kanser otak. Kajian yang dilakukan oleh Wang dan rakan-rakan telah
melaporkan bahawa artesunat memekakan sel kanser ovari terhadap cisplatin
melalui pengawalan rendah RAD51, protein yang membaiki pecahan rantai ganda
DNA, dan menghalang pembentukan klonogenik sel kanser tersebut. Selain itu,
kajian oleh Hou dan rakan-rakan telah melaporkan bahawa tanpa mengira status
p53 dalam sel hepatoma, artemisinin, dan derivatifnya terbukti sebagai agen
kemosensitisasi yang kuat. Kajian ini telah disokong oleh banyak kajian lain
yang telah melaporkan artemisinin sebagai agen kemosensitisasi.
Terdapat pelbagai laporan penyelidikan yang
telah mendapati artesunat dapat menjalankan aktiviti antikanser. Artesunat ialah
artemisinin semisintetik larut air dengan sifat farmakokinetik yang lebih baik
dan telah disyorkan oleh Organisasi Kesihatan Sedunia sebagai rawatan utama
untuk malaria. Walaupun mekanisme artesunate dalam menghalang pertumbuhan
kanser tidak difahami sepenuhnya, namun terdapat teori yang mencadangkan besi
ferus merangsang pembentukan radikal sitotoksik. Kajian sebelum ini telah
menunjukkan bahawa menyekat reseptor transferrin dalam sel karsinoma
hepatoselular oleh antibodi monoklonal tertentu dapat membatalkan aktiviti antikanser
artesunat. Oleh kerana hati berfungsi sebagai tempat pengumpulan besi,
metabolisme artesunat sangat aktif dalam hepatosit. Tambahan pula, pertumbuhan sel
karsinoma hepatoselular memerlukan metabolisme besi yang tinggi, dan menunjukkan
peningkatan ekspresi reseptor transferrin. Oleh kerana reseptor transferrin
bertanggungjawab untuk pengambilan dan pengawalan besi intrasel, artesunat
mungkin mempunyai keberkesanan yang lebih besar dalam sel karsinoma
hepatoselular.
Secara amnya, mekanisme antikanser oleh derivatif
artemisinin yang telah dilaporkan termasuklah induksi apoptosis melalui
penjanaan spesis oksigen reaktif, kesan perencatan angiogenesis, perencatan
pengaktifan faktor-1? (HIF-1?) yang boleh disebabkan oleh hipoksia oleh
penjanaan ROS, dan kecederaan DNA langsung. Menariknya, Eling dan rakan-rakan
telah melaporkan bahawa artesunat telah mengaktifkan feroptosis dalam sel
adenokarsinoma pankreas. Singh dan Verma telah melaporkan kes pesakit dengan
karsinoma laring sel skuamosa. Pesakit telah dirawat selama lima belas hari
dengan 60 mg dos intramuskular artesunat setiap hari diikuti dengan 50 mg
artemisinin oral selama sembilan bulan. Selepas dua bulan rawatan, mereka
melaporkan pengurangan sebanyak 70% tumor, serta pemulihan drastik disfagia dan
disfonia pesakit. Dalam ujian klinikal yang dijalankan oleh Zhang dan rakan-rakan,
121 pesakit kanser paru-paru bukan sel kecil telah dikaji. Satu kumpulan
menerima rawatan konvensional vinorelbine dengan cisplatin manakala kumpulan
kedua menerima rawatan yang disebutkan sebelum ini ditambah artesunat intravena
selama lapan hari. Pemerhatian menunjukkan peningkatan kawalan penyakit dalam
kumpulan yang menerima rawatan konvensional bersama artesunat sebanyak 88.2% berbanding
kumpulan yang menerima rawatan konvensional sahaja iaitu sebanyak 72.7%. Ini
memberi gambaran bahawa artesunat mempunyai kesan antikanser yang memberangsangkan.
Namun begitu, penyelidikan yang lebih terperinci perlu dilaksanakan untuk
membuktikan keberkesanan artesunat sebagai antikanser. Aplikasi artesunat sebagai
antikanser memberi kelebihan kerana sifat kimia serta tindakbalas farmakologi
telah diketahui dan dilaporkan sejak berpuluh tahun dahulu.
1. Vandewynckela Y, Laukensa L, Geertsa A, Vanhoveb C, Descampsb B, Collea I, Devisschera L, Bogaertsa E, Paridaensa A, Verhelsta X, Van Steenkistea C, Libbrechte L, Lambrecht BN, Janssensc S, Van Vlierberghea H (2014). Therapeutic effects of artesunate in hepatocellular carcinoma: repurposing an ancient antimalarial agent. European Journal of Gastroenterology & Hepatology, 26: 8.
2. Yao Y, Guo Q, Cao Y, Qiu Y, Tan R, Yu Z, Zhou Y, Lu N (2018). Artemisinin derivatives inactivate cancer associated fibroblasts through suppressing TGF-? signaling in breast cancer. Journal of Experimental & Clinical Cancer Research, 37:282
3. Wang B., Hou D., Liu Q., Wu T., Guo H., Zhang X., Zou Y., Liu Z., Liu J., Wei J., et al (2015). Artesunate sensitizes ovarian cancer cells to cisplatin by downregulating RAD51. Cancer Biol. Ther, 16:1548–1556.
4. Hou J., Wang D., Zhang R., Wang H (2008). Experimental therapy of hepatoma with artemisinin and its derivatives: In Vitro and in vivo activity, chemosensitization, and mechanisms of action. Clin. Cancer Res, 14:5519–5530.
5. Sun X, Ou Z, Chen R, Niu X, Chen D, Kang, R, Tang D (2015). Activation of the p62-Keap1-NRF2 pathway protects against ferroptosis in hepatocellular carcinoma cells. Hepatology, 63(1):173-84.
6. Eling N, Reuter L, Hazin J, Hamacher-Brady A, Brady NR (2015). Identification of artesunate as a specific activator of ferroptosis in pancreatic cancer cells. Oncoscience, 2:5.
7. Zhang P., Luo H.S., Li M., Tan S (2015). Artesunate inhibits the growth and induces apoptosis of human gastric cancer cells by downregulating COX-2. OncoTargets Ther, 8:845–854.
Penulis Artikel
Dr Nor Hazwani Ahmad
Afiliasi:
Kluster Sains Onkologi dan Radiologi, IPPT, USM
Bidang kepakaran:
Biologi Kanser

Siti Nazmin binti Saifuddin dan Sharlina binti Mohamad
Kluster Perubatan Integratif, Institut Perubatan dan Pergigian Termaju (IPPT), USM
Kanser merupakan beban utama
penyakit di seluruh dunia dan menimbulkan cabaran besar kedua-duanya kepada pakar
perubatan dan penyelidik ekoran etiologi dan mekanisme sebenar penyakit ini
masih samar. Menurut laporan kedua yang dikeluarkan oleh Pendaftaran Kanser
Kebangsaan Malaysia (MNCR), sebanyak 115,238 kes kanser baharu telah didaftarkan
di negara ini bagi tempoh 2012-2016 berbanding 103,507 kes yang dilaporkan
dalam laporan pertama yang merangkumi tempoh 2007-2011. Peningkatan kes yang ketara
ini turut mencerminkan peningkatan kos-kos lain yang perlu ditanggung oleh
semua pihak yang terlibat baik pesakit, keluarga, mahupun negara.
Di Malaysia, kadar kejadian
kanser dalam kalangan wanita adalah lebih tinggi berbanding lelaki. Sepuluh
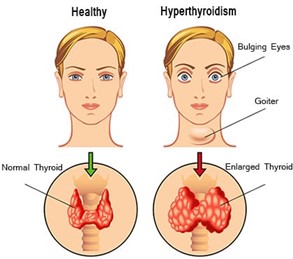
kanser paling biasa yang dilaporkan dalam kalangan wanita adalah kanser payudara,
kolorektal, serviks uteri, ovari, paru-paru, korpus uteri, limfoma, tiroid,
leukemia dan kulit (bukan melanoma); manakala dalam kalangan lelaki pula adalah
kanser kolorektal, paru-paru, prostat, limfoma, nasofaring, hati, leukemia, perut,
kulit (bukan melanoma) dan pundi kencing. Meskipun terdapat program saringan
untuk sesetengah jenis kanser, namun peningkatan kes yang ketara jelas
menunjukkan kepentingan langkah pencegahan yang berkesan, pengesanan awal dan
peningkatan kesedaran awam dalam mengawal penyakit ini.
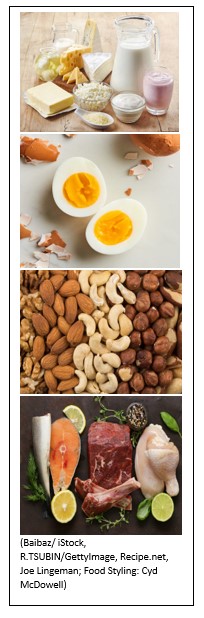
Selain daripada faktor genetik, faktor luaran merupakan penyebab utama pembentukan kanser. Antara punca yang dikaitkan dengan kanser adalah tabiat pemakanan termasuk jenis-jenis makanan dan cara penyediaannya, gaya hidup dan aktiviti fizikal, berat badan dan pengambilan alkohol. Berikut adalah antara langkah-langkah pencegahan yang disarankan oleh World Cancer Research Fund bagi mencegah kanser:
Sharlina Mohamad dan Siti
Nazmin Saifuddin
Kluster Perubatan
Integratif, Institut Perubatan dan
Pergigian Termaju (IPPT), USM
Kanser merupakan salah satu punca utama kematian di seluruh dunia. Dalam kalangan negara-negara Asia sahaja, kes kanser dianggarkan meningkat daripada 1.6 juta pada tahun 2008 kepada 10.7 juta pada tahun 2030, dengan kanser paru-paru mencatatkan kes tertinggi bagi lelaki, dan kanser payudara bagi wanita.
Metastasis kanser dalam tulang menyebabkan
kesakitan yang sederhana hingga sangat teruk kepada pesakit. Sakit kronik pada
tulang ini perlu ditanggung oleh pesakit secara berterusan. Walaupun tulang
bukanlah organ vital dalam badan manusia, namun terdapat pelbagai kanser seperti
payudara, prostat, tiroid, buah pinggang, dan paru-paru, yang cenderung untuk
bermetastasis ke beberapa bahagian tulang.
Kebanyakan kesakitan tulang
malignan disebabkan metastasis pada tulang adalah bermula dari kanser payudara
dan prostat. Pada permulaannya, kesakitan tulang disebabkan kanser ini dirasai dalam
sela masa tertentu, namun kesakitan ini akan berkembang dengan cepat dan berterusan,
yang diburukkan lagi oleh episod kesakitan yang tidak tertanggung.
Sebaik sahaja kesakitan kronik
ini dialami oleh pesakit, keadaan akan menjadi semakin buruk apabila allodynia
mekanikal berlaku. Allodynia mekanikal adalah keadaan apabila aktiviti atau
rangsangan yang biasanya tidak menyakitkan dirasakan sangat menyakitkan. Contohnya
pergerakan ringkas seperti batuk, memusingkan badan di atas katil, atau pergerakan
anggota badan yang perlahan, akan menyebabkan kesakitan yang teruk.
Intervensi semasa
Terdapat pelbagai kaedah yang
digunakan untuk merawat kesakitan disebabkan kanser tulang ini, seperti rawatan
menggunakan “bisphosphonate”, kemoterapi, pembedahan, sekatan saraf,
imunoterapi, dan penyingkiran gen. Rawatan menumpukan pada program tiga langkah,
yang ditetapkan oleh Pertubuhan Kesihatan Sedunia (WHO). Mengikut tahap
kesakitan, pesakit akan diberikan analgesik anti-radang bukan steroid (untuk sakit
ringan) dan/atau terapi opioid (untuk sakit sederhana dan teruk). Namun kebanyakan
sakit tulang yang dialami kebanyakan pesakit masih tidak dapat dihentikan
sepenuhnya, dan terdapat banyak kesan ubatan yang perlu dihadapi selepas
rawatan menggunakan ubatan di atas, seperti toleransi morfin, sembelit, depresi
respiratori disebabkan ubat opioid, serta ulser perut dan ketoksikan buah
pinggang yang disebabkan oleh analgesik anti-radang bukan steroid. Penggunaan
ubat-ubatan ini dihadkan oleh kesan-kesan sampingan ini.
Kajian berterusan diperlukan bagi
membantu pesakit-pesakit kanser yang telah mengalami metastasis ke tulang ini
mengurangkan kesakitan yang mereka alami dan memberi keselesaan buat mereka
menjalani kehidupan.




















Dr. Noor Khairiah A. Karim
Kluster Perubatan Regeneratif, Institut Perubatan dan Pergigian Termaju, Universiti Sains Malaysia
Penyakit arteri koronari atau coronary arterial disease (CAD) berlaku disebabkan pembentukan plak atau aterosklerosis yang terbentuk daripada kolesterol, kalsium, dan bahan pembekuan darah pada dinding salur darah arteri koronari yang menyempitkan arteri tersebut dan boleh mengakibatkan pengurangan pengaliran darah yang membekalkan oksigen dan nutrien kepada jantung. Susulan komplikasi ini, seseorang boleh mengalami gejala seperti sakit dada dan kesesakan nafas. Proses penyempitan arteri ini mengambil masa yang agak lama maka seseorang individu itu pada umumnya hanya akan menyedari bahawa beliau menghidap CAD apabila berlakunya serangan jantung terutamanya apabila arteri koronari ini tersumbat sepenuhnya.
Faktor Risiko
Terdapat pelbagai faktor yang berupaya menyumbang kepada CAD. Ini termasuk faktor umur, jantina, mempunyai sejarah keluarga yang menghadapi serangan jantung, menghidap tekanan darah tinggi dan penyakit kencing manis, tahap kolesterol yang tinggi, obesiti, merokok, kurang bersenam, stres dan pengambilan diet yang tidak atau kurang sihat.
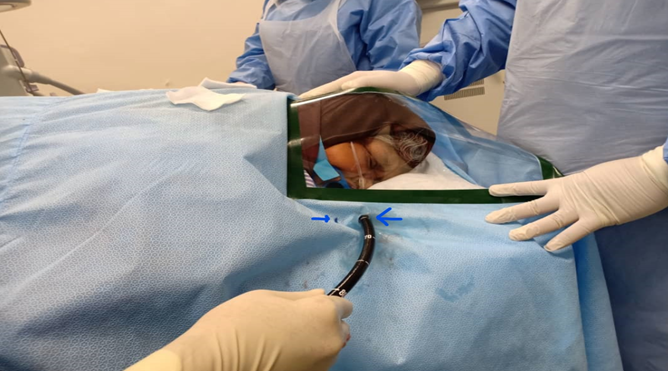
Peranan Imbasan Tomografi Berkomputer
Saringan awal CAD dapat dilakukan dengan menjalankan pemeriksaan imejan. Lazimnya, pakar perubatan akan mencadangkan pemeriksaan skor kalsium atau calcium scoring kepada pesakit yang berisiko mendapat CAD. Calcium scoring merupakan pemeriksaan bukan invasif yang menggunakan imbasan tomografi berkomputer atau computed tomography (CT) untuk mengenalpasti keberadaan, kedudukan dan tahap kalsifikasi di dalam salur arteri koronari bagi menentukan kadar risiko seseorang berkemungkinan menghidap CAD.
Semasa pemeriksaan ini dijalankan, yang lazimnya hanya mengambil masa kurang daripada 5 minit, elektrokardiografi akan dipasang pada dada pesakit dan aktiviti serta kadar denyutan jantung akan dipantau. Pesakit perlu berada dalam keadaan selesa dan tenang, dan berupaya mengikut arahan yang diberikan bagi memastikan kadar denyutan jantung berada dalam keadaan stabil dan imej yang optimum dapat diperoleh untuk memudahkan proses analisis. Seterusnya, kadar kalsium di dalam salur darah arteri koronari akan diukur dan peratusan plak akan dikira secara automatik. Skor Agatston ialah alat separa automatik untuk mengira skor berdasarkan tahap kalsifikasi arteri koronari yang dikesan oleh imbasan CT dos rendah ini yang secara rutin dilakukan pada pesakit yang menjalani CT jantung. Stratifikasi risiko awal dapat dijalankan kerana pesakit dengan skor Agatston yang tinggi (>160) mempunyai peningkatan risiko untuk serangan jantung yang serius.
Secara umumnya, hasil calcium scoring dan risiko CAD diklasifikasikan seperti di bawah:
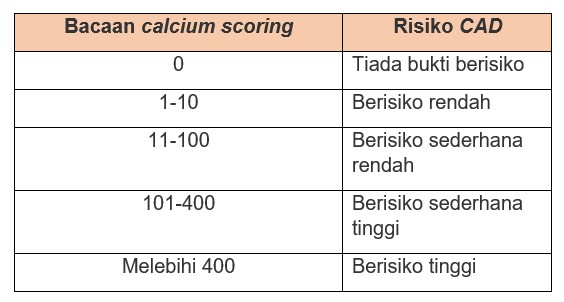
Untuk individu yang mempunyai bacaan negatif iaitu 0 dan 1-10 (berisiko rendah), kebarangkalian untuk mendapat CAD dalam tempoh 2 sehingga 5 tahun akan datang adalah sangat rendah. Individu yang mempunyai skor 1-10 dan 11-100 iaitu yang berisiko rendah dan sederhana rendah lazimnya dinasihatkan untuk mengamalkan gaya hidup sihat daripada segi pengambilan makanan dan juga aktiviti harian. Untuk individu yang berisiko sederhana tinggi iaitu bacaan 101-400, rawatan dan pemeriksaan lanjut diperlukan kerana kemungkinan berlakunya kejadian arteri koronari tersumbat sepenuhnya yang menyebabkan berlakunya serangan jantung adalah sangat tinggi. Manakala bagi individu yang mempunyai bacaan melebihi 400, kebarangkalian berlakunya kejadian arteri koronari tersumbat sepenuhnya ialah 90%. Justeru itu, rawatan lanjut amat diperlukan dan ini termasuk prosedur invasif.
Perjumpaan secara berkala dengan pakar terutamanya bagi pesakit berisiko sederhana tinggi dan tinggi adalah sangat penting bagi meneliti sebarang perubahan yang serius pada jantung dan memastikan keberkesanan ubat-ubatan yang diambil. Pada ketika ini, pakar akan memberi ubat-ubatan yang perlu diambil serta menekankan langkah-langkah pencegahan yang perlu dilakukan oleh pesakit bagi mengurangkan risiko mendapat serangan jantung. Ini termasuklah amalan gaya hidup dan pengambilan makanan yang sihat.
Penulis
Dr Noor Khairiah A. Karim
Pensyarah Perubatan dan Pakar Radiologi
Kluster Perubatan Regeneratif, Institut Perubatan dan Pergigian Termaju, Universiti Sains Malaysia


